Abstract
Background: The more painful cause of excruciating anal pain is anal fissures. An anal fissure, known as a fissure-in-ano, is a vertical split that runs from the anal margin proximally to the dentate line but does not go past it.
Aim: Compare the fissure healing process and side effects of a smooth muscle relaxant, topical treatment 2% diltiazem gel, with lateral internal anal sphincterotomy (LIS) in the treatment of chronic anal fissures.
Materials and Methods: Random controlled trial was dine in Surgical unit Samarra General Hospital, from October 2018 to August 2019 with 6 months follow-up. The study included 60 cases chronic anal fissure surgery outpatients and/or hospitalized patients were randomly grouped into one of two groups: Group A (topical Diltiazem gel) or Group B (lateral internal sphincterotomy operation), with 30 patients in each.
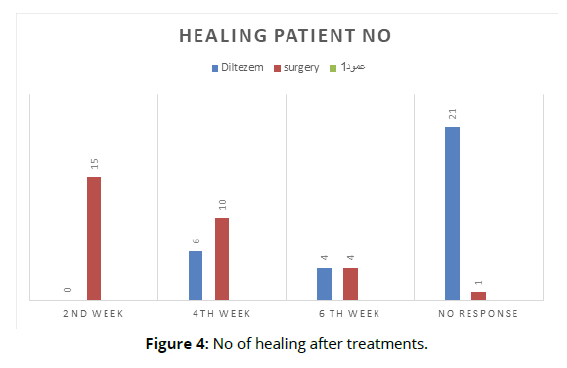
Results: Patients were checked on every week for a six weeks in a row, after that every two weeks for the next three weeks were healed, followed by ten at 4 weeks and five at 6 weeks. 20 patients with group A and 1 patient with group B did not heal. The overall healing rate in this trial was 32% with diltiazem and 98 % with lateral internal anal sphincterotomy operation after 6 weeks (LIS).
Conclusion: It has been determined that lateral internal sphincterotomy is superior to 2% diltiazem gel.
Keywords
Chronic anal fissures. Diltiazem. Lateral internal sphincterotomy operation
Introduction
The more painful cause of excruciating anal pain is anal fissures. An anal fissure, known as a fissure-in-ano, is a vertical split that runs from the anal margin proximally to the dentate line but does not go past it. [1] It typically starts at the level of the dentate line and extends to the anal verge in the posterior or anterior midline. Within three to six weeks of the commencement of symptoms, an acute fissure manifest. Anoderm appears to have been cleanly torn longitudinally, with little surrounding inflammation. Within six weeks, an acute fissure typically spontaneously heals. With symptoms lasting longer than six weeks, a fissure was typically deeper and it exposed internal sphincter fibers at its basement. It usually has a sentinel pile at its distal aspect and a hypertrophy anal papilla on its upper aspect. It is categorized as primary (idiopathic) or secondary according on the etiology. Secondary fissures are those that develop as a result of another pathology, such as AIDS, anal TB, or Crohn's disease. Patients typically present with pain during feces and bright red blood passing through the anus. Anal fissure's precise etiology is unknown. The most frequent cause of fissure is trauma caused by the passage of a large, hard stool (constipation), although it can also occur after a bout of acute diarrhea and after childbirth 2. Painful fissures are frequently accompanied by uncontrollable internal sphincter spasms and excessive anal canal rest pressure. Therefore, it appears that chronic overactivity of the internal sphincter may be the reason. Normal resting anal pressure ranges from 80 to 160 mm Hg 3. Anal soreness after urination is a symptom of an anal fissure. The skin in the lower portion of the fissure might swell in chronic situations and serve as a "sentinel pile," or sign, for an anal fissure. [8] Anal sphincter spasm reduction improves blood flow and speeds up wound healing. The majority of fissures are effectively repaired by surgical procedures such lateral internal sphincterotomy or manual anal dilatation within a few weeks 4,5, although they may cause permanently compromised anal continence. This prompted studies on non-surgical alternatives 6, and it has been demonstrated that a number of pharmacological medications, including nitrates (glyceryl trinitrate) and calcium channel blockers (diltiazem), can reduce anal pressure and treat fissures without endangering incontinence. 7. Aim: Compare the fissure healing process and side effects of a smooth muscle relaxant, topical treatment 2% diltiazem gel, with lateral internal anal sphincterotomy (LIS) in the treatment of chronic anal fissures
Materials and Methods
The study is done in Samarra General Hospital surgery department. The study was done between October 2018 and August 2019 with 6-month follow-up. After receiving written informed consent, a total of 60 patients were enrolled in the study. They were then divided into two groups of 30 patients each at random. The study covered both sexes and all clinically diagnosed individuals with chronic anal fissures between the ages of 15 and 60. Patients with hemorrhoids, signs of a fistula, a fungating mass, or advanced anal canal cancer, patients with rectal prolapse, fissures caused by specific diseases like tuberculosis, Crohn's disease, etc., pregnant women, and people with hypersensitivity to calcium channel blockers were all disqualified from participating. The length of the pain, along with other related symptoms including constipation, rectal bleeding, discharge and soiling, sentinel pile, and previous treatments received, were all noted in the thorough history that was recorded. All of the information was carefully examined and entered into forma. Chronic anal fissures were defined as fissures that did not heal within six week despite simple food changes, fissures with tough borders, and fissures without healing tissue with sign of skin tag, hypertrophied papilla. Patients were told to apply a pea-sized amount of the 2% Diltiazem to the anal margins and gently rub them for 5-8 seconds in a clockwise direction. A tiny amount was also placed at least 1.5 cm into the anus. For six weeks, the ointment was used twice every day. Before and after using the ointment, patients were instructed to wash their hands. At the second, fourth, sixth, and twelfth weeks, all patients underwent outpatient reviews. Lateral internal sphincterotomy was performed on group B patients. Under general or regional anesthesia, an open lateral internal anal sphincterotomy was carried out (spinal or caudal). Under direct vision, the internal sphincter is divided after the radial incision at the anoderm is made above the intersphincteric groove. An area of the internal anal sphincter that measured about 2 cm long was split. By applying lateral pressure with the finger to the innermost muscle fibers, the integrity of the mucosa was preserved. Pressure was held for two to three minutes in order to achieve hemostasis. Sphincterotomy patients were not given any additional treatments or topical ointments. Patients received no prophylactic antibiotic and were released after 24 hours. Cases from both groups were instructed to consume a high-fiber diet and moderate laxatives. Patients were observed every two weeks for a total of six weeks, during which time the fissures were checked for healing and the two treatments' adverse effects-headache in group A and bleeding, infection, uncontrolled to feces and flatus in group B-were assessed. Patients with an epithelium-covered fissure that had fully healed were deemed to be in remission. During follow-up, post-treatment incontinence for feces and flatus was assessed by an impartial observer every two weeks. Age, time, and other quantitative characteristics were provided as standard deviation. By using the Chi-square with a p.p 0.05 level of significance for males, the hypothesis was evaluated
Results
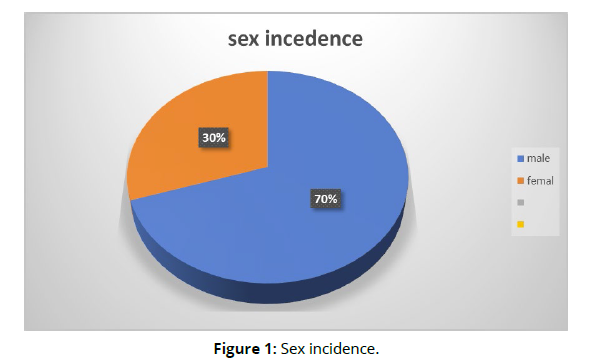
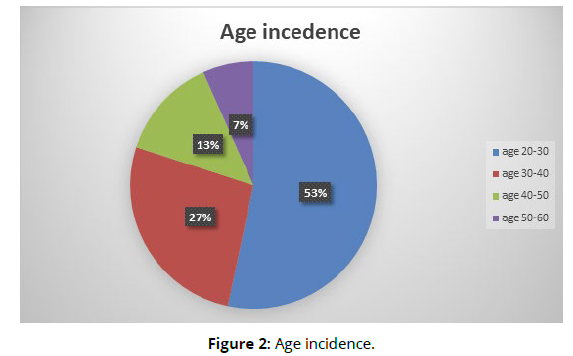
Out of 60 patients 42 cases (70%) man and 18 cases (30%) women (Figure 1). The man-to-women ratio was 2.3:1 (Figure 2), with an age range from 15-60 years. The mean for age was 33.521+ 4.55 years.
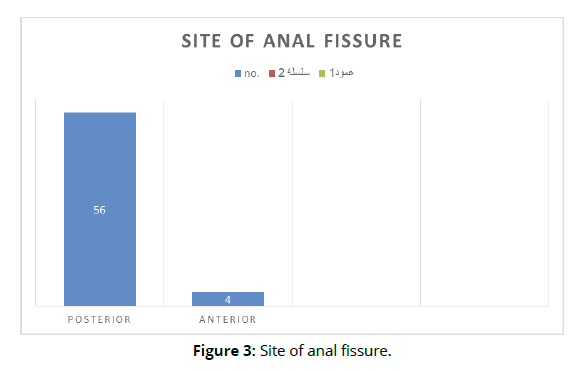
Clinical features in those patients were pain in defecation and non absolute constipation in all 60 cases, bleeding from rectum in 55 cases, mucus discharge in 26, sentinel pile gaurd in 32, and pruritus in anus in 11 patients. In this study 56 (93%) patients had posterior midline fissures and 4 (6%) had anterior midline fissures (Figure 3).
Table 1 show the number of pains relives after diltiazem treatment and after surgery, after 2, 4, 6 weeks, and also several patients with persistent pain. In group A, six cases with healed of fissure after 4 weeks and in subsequent 4 at 6th week. In group B 15 cases had healed at 2 weeks and in subsequent 10 at 4 weeks and 4 cases at 6 weeks (Table 1). One case in group B and 20 cases in group A had no healing. A Chi-square test was applied to test the significance of healing in both groups. P-value was calculated and was found to be > 0.05. Regarding complications, headaches occurred in 5 (16.6%) patients using diltiazem gel, whereas none of the surgery group had this problem. The pain was transient and did not require any treatment. Incontinence was seen in one (3.3%) patient in the surgery group. Other complications like post-operative bleeding and infection were not seen in the surgery group (Figure 4).
| Group B (surgery LIS) | Group A (Diltiazem) | No .of pain relievers patients |
|---|---|---|
| 18 | 14 | At end of 2nd week |
| 12 | 10 | At end of 4th week |
| 4 | 4 | At end of the 6th week |
| 0 | 3 | Persistence of pain |
Discussion
Anal fissures are a fairly prevalent issue that significantly reduces the comfortability of life and causes significant morbidity. Condition needs to be treated right away using the proper techniques. Numerous theories have been put forth over the years regarding how anal fissures occur. The underlying causes have been hypothesized to range from anal injuries to internal sphincter hypertonia and subsequent local ischemia resulting in no recovery.
5,6 Anal fissures may manage in a many different ways, including surgical and pharmaceutical procedures. The main goal of treatment, regardless of the approach, to decrease the tonicity of the internal anal sphincter, which will boost regional blood flow and eventually promote healing at the injured area. Anal fissures are now approved at many clinics as the first line of treatment with chemical sphincterotomy, a medical procedure. Diltiazem show to be of value in management of anal fissures in studies past. The pharmacological drugs used include calcium channel blockers (nifedipine, diltiazem), nitrates (isosorbide dinitrate or glyceryl trinitrate), botulinum toxin, alpha adreno antagonist and agonists, and muscarinic receptor agonists. Additionally investigated are more recent substances like gonyautoxin, a neurotoxic that causes paralysis. Lateral internal sphincterotomy, one of the surgical procedures, is now recognized as the gold standard. 3 Other surgical techniques include fissurectomy and fissurotomy techniques, local flap techniques like V-Y advancement flaps and rotation flaps,9,10, and sphincterolysis,11 calcium channel blockers mode of it action is by blocking L- channels, lead toth muscle relaxation and lowering anal tone. However, the benefit of diltiazem cream is temporary in some patients. In other investigations, the healing rates of chronic anal fissures ranged from 47% to 89%,13–17 while the rate found in our study is 33.3%. The short followup period in our study may have contributed to this outcome (6 weeks). While in their study, Knight et al. found that only one patient out of 71 suffered a headache. 17 However, we found 5 (16.6%) patients to have headaches. Many surgeons prefer to treat anal fissures using lateral sphincterotomy. Under either local or general anesthesia, it can be carried out using either an open or a subcutaneous approach. Minor complications such as pruritus, chronic wound pain, bleeding, abscess, discharge, urgency, impaction, or deficiency of continence were observed in the literature. Major complications necessitating reoperation included bleeding, fistula, abscess, or an unhealed wound. 18 Only one patient (3.33%) with incontinence was identified in our investigation.
Conclusion
Anal fissures are a frequent issue. The management's main goal is to lower anal pressures. With few adverse effects and modest cure rates, anal fissures can typically be treated with conservative therapy/pharmacologic care using topical calcium channel blockers. Because of its simplicity, superior healing rates, higher patient satisfaction, little morbidity, and low complication rates, lateral internal sphincterotomy continues to be the gold standard for the permanent therapy of anal fissures.
References
Lunniss PJ. The anus and anal canal. In: Williams NS, Bulstrode CJK, O’Connell PR. Bailey & Love’s Short Practice of Surgery. 25th ed: London, Arnold, 2008:1251- 3.
Herzig DO, Lu KC. Anal fissure. Surg Clin North Am 2010;90:33-44.
Goligher John, Anal Fissure, John Goligher. Surgery of the Anus, Rectum & Colon.AITBS.(5th Edition) 1992:150.
Bharadwaj R, Parker MC. Modern perspectives in the treatment of chronic anal fissures. Ann R Coll Surg Engl 2007; 89: 472- 8.
Van Outryve M. Physiopathology of the anal fissure. Acta Chir Belg 2006;106: 517-8.
Jonas M, Scholefield JH. Anal fissure. Gastroenterol Clin North Am 2001; 30:167- 81.
Pelta AE, Davis KG, Armstrong DN. Subcutaneous fissurotomy: a novel procedure for chronic fissure-in-ano. A review of 109 cases. Dis Colon Rectum 2007; 50: 1662-7.
Kumar Y, Kumar P. Lateral Internal Sphincterotomy Versus 2% Diltiazem Gel Local Application: A Comparative Study in Treatment of Chronic Fissure in Ano. Indian J Appl Res 2018:8.
Singh M, Sharma A, Gardiner A, Duthie GS. Early results of a rotational flap to treat chronic anal fissures. Int J Colorectal Dis 2005; 20: 339-42.
Giordano P, Gravante G, Grondona P, Ruggiero B, Porrett T, Lunniss PJ. Simple cutaneous advancement flap anaplasty for resistant chronic anal fissure: a prospective study. World J Surg 2009; 33: 1058-63.
11 Nash GF, Kapoor K, Saeb-Party K, Kunanadam T, Dawson PM. The long-term results of Diltiazem treatment for anal fissure.International Journal of Clinical Practice.2006; 60(11):1411–13.
Griffin N, Acheson AG, Jonas M, Scholefield JH. The role of topical diltiazem in the treatment of chronic anal fissures that have failed glyceryl trinitrate therapy. 2002; 4: 430- 5.
Kocher HM, Steward M, Leather AJ, Cullen PT. A randomized clinical trial assessing the side effects of glyceryl trinitrate and diltiazem hydrochloride in the treatment of chronic anal fissure. Br J Surg 2002; 89: 413-7.
Jonas M, Speake W, Scholefield JH. Diltiazem heals glyceryl trinitrate-resistant chronic anal fissures: a prospective study. Dis Colon Rectum 2002; 45: 1091-5.
Carapeti EA, Kamm MA, Phillips RK. Topical diltiazem and bethanechol decrease anal sphincter pressure and heal anal fissures without side effects. Dis Colon Rectum 2000; 43: 1359-62.
Kocher HM, Steward M, Leather AJ, Cullen randomized mixed clinical trial assessing the side-effects of glyceryl trinitrate and diltiazem hydrochloride in the treatment of chronic anal fissure. Br J Surg 2002; 89: 413-7.
Knight JS, Birks M, Farouk R. Topical diltiazem ointment in the treatment of chronic anal fissure. Br J Surg. 2001; 88: 553-6.
Richard CS, Gregoire R, Plewes EA. Internal sphincterotomy is superior to topical nitroglycerin in the treatment of chronic anal fissure: Results of a randomized, controlled trial by the Canadian Colorectal Surgical Trials Group. Dis Colon Rectum 2000; 43: 1048-58.
Author Info
1Department of surgery, Collage of medicine, Tikrit University, IraqReceived: 05-Jan-2023 Accepted: 06-Feb-2023 Published: 13-Feb-2023