Cyclosporine Nephrotoxicity in Patients with Type 1 Diabetes Mellitus Arbitrary Verdict: A Meta-Analysis of Randomized Control Trials
Abstract
Background: Disturbance in renal function was considered to be a common complication of Cyclosporine-A (CsA) treated patients of recent-onset type 1 diabetes mellitus, for purposes of remission. The aim of the present study was to scrutinize the potential association between this drug and its complications by conducting a meta-analysis of randomized control trials.
Methods: A consummate literature search of PubMed, EMBASE, and web of science was conducted until March 2019. A total of 9 randomized control trials were included in this meta-analysis.
Results: On meta-analysis of nine studies evaluating the risk of transient complications, analysis of the random effect of 12 months-low dose-cyclosporine on serum creatinine, revealed the absence of CsA induced nephrotoxicity. And no association between CsA and renal function in newly diagnosed type 1 diabetic patients Odds Ratio (OR), 1.06; 95% Confidence Interval (CI), 1.00-1.43; I2=73.1%). No noteworthy publication bias was noticed in the designated 9 studies.
Conclusion: 12 months low dose CsA was not associated with risk of deterioration of renal function according to the results revealed from the meta-analysis of RCTs which is considered as the summit of the research pyramid.
Keywords
Cyclosporine • Renal function • Type 1 diabetes mellitus • Meta-analysis
Abbreviations
RCT=Randomized Control Trial; CsA=Cyclosporine A; CI=Confidence Intervals; NOS=Newcastle-Ottawa Scale; OR=Odds Ratios; PRISMA=Preferred Reporting Items for Systematic Reviews and Meta-Analyses; OR=Odds Ratio; RR=Relative Risk; T1DM=Type 1 Diabetes Mellitus; MOOSE=Meta-Analysis of Observational Studies in Epidemiology
Introduction
Cyclosporine A (CsA) Short-term treatment improves the rate of clinical remission in recent onset type 1 insulin-dependent diabetes mellitus. It is recognized, however, that the usage of CsA is linked to the associated modification in kidney functions. Erstwhile studies have publicized that nephrotoxicity is not only restricted to patients with kidney transplantation. In almost all studies implemented among patients of kidney or heart transplantations, to the side of patients with autoimmune disorders like rheumatoid arthritis, primary biliary cirrhosis, psoriasis or uveitis, a substantial loss in kidney function was witnessed throughout longterm CsA administration [1]. Our designated researches were accomplished in recent-onset type I diabetic patients to evaluate the alterations in kidney function concomitant with a lowmoderate dose of CsA and to assess its ultimate efficacy to return to normal after termination of this immunosuppressive drug. The first published research assessed the effect of cyclosporine on renal function in diabetic patients was performed in 1985. And the last one was in 2002. Same leader and different teams. However, up till this moment no meta-analyses or systematic reviews were done to establish statistical significance across studies that might otherwise seem to have conflicting results. This will increase the validity and reliability of information and any observed differences. Our drive was to examine the relationship between CsA and the subsequent complications in diabetic patients participating in randomized control trials [2].
Materials and Methods
We reported this systematic review and meta-analysis according to the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). We also conducted this work based on the Meta-Analysis of Observational Studies in Epidemiology (MOOSE) there was no need for involvement of institutional review board or ethics commission agreement as there was no patient participation.
Formulation of the research question
Research question was focusing on and fulfilled the main pillars to start conduction of meta-analysis, in terms of population, intervention/ exposure, comparison groups, outcome of interest, time of study, follow up duration and place of study. The question was what is the effect of low and moderate doses of cyclosporine A on renal function? particularly the level of serum creatinine among newly diagnosed patients with type 1 diabetes mellitus [3]. Cyclosporine was given for remission and restoration of beta cell function, as studied in previous RCTs conducted in Europe and North America in different countries. The outcome was kidney function deterioration. The five elements were fulfilled also; nephrotoxicity as a domain, serum creatinine level as a specific measurement and specific metric of normal creatinine value which was 0.6 to 1.2 milligrams (mg) per deciliter (dL) in adult males and 0.5 to 1.1 milligrams per deciliter in adult females. And 0.5 to 1.0 mg/dL for children ages 3 to 18 years, 0.3 to 0.7 mg/dL for children under age 3. All selected studies used Cockcroft-Gault equation to estimate the identifiable level of serum creatinine denoting nephrotoxicity, through creatinine clearance. Creatinine clearance=((140-age) × weight in kg)/(serum creatinine × 72). We used multiple methods of aggregation like means, SE and P value. All of these values were easily abstracted from available trials, apart from what was needed to be statistically calculated outside. For period of studies and time points of follow up, most of studies followed their patients and investigated them at fixed stations of time (3, 6, 8, 9, 12 and 24 months) [4].
Search strategy
Hand searching of major bibliographic databases and key electronic databases in the form of controlled vocabulary indexing of Randomized Controlled Trials (RCTs) MEDLINE/PubMed, EMBASE, Cochrane Central Register of Controlled Trials (CENTRAL), LILACS, CINAHL, Psych INFO, OTSeeker, Web of Science, Scopus, Dissertations, thesis databases, Gray literature databases and FDA were searched using selected key words regarding Cyclosporine (CsA) and Type 1 Diabetes Mellitus (TIDM) (last search update, March 2019). Key words were characterized by consistency, alternative spellings, synonyms, plurals and related terms. The key word group for cyclosporine was composed by immunosuppressant medication, calcineurin inhibitors, Ciclosporinum, nephrotoxicity, glomerular filtration rate, renal plasma flow, renal vascular resistance, creatinine clearance, type 1 diabetes, juvenile diabetes and urinary sodium excretion. No limitations of linguistic or publication records in literature exploration were smeared. In addition, the references of the searched articles were appraised to recognize other eligible researches (snow ball tracing). When additional data were necessary, the approach with the main authors of related articles was conducted if needed [5].
Inclusion and exclusion criteria
In terms of inclusion, an article would be counted in if it met the subsequent criteria: A clear correlation between the effect of cyclosporine on renal function in patients with type 1 diabetes mellitus was evaluated; a RCT study design was adopted; the Relative Risk (RR), Odds Ratios (OR), with 95% Confidence Intervals (CI) or adequate data to compute, analyze and estimate them were testified. The exclusion criteria comprised: Not RCT design was implemented; no available data in appropriate presentation was conveyed. We exclude all other study designs even though they targeted our goal precisely. Because results from different study designs should be expected to differ systematically, resulting in increased heterogeneity. We exclude prospective cohort studies because they did not contain associations, OR, RR or CI, just descriptive statistical data. However, CI and P-values have been statistically calculated from means and standard errors in some selected studies [6].
Data extraction and quality scale
Two interrogators (AE and AE) hauled out the data from each encompassed publication autonomously. The data extracted comprised the name of the corresponding author of each publication, country where the study done, participants’ age, period of study, year of publication, definition of exposure, matched or adjusted factors, OR/RR values in each study. If together adjusted and non-adjusted data were displayed, simply the adjusted values were deployed. We extracted and deployed only the highest and the lowest values in data groups to be used in calculation, in case of presence of stratified or clustered data in the original study. We used the subsequent mathematical formula to calculate relative risk in main and subgroup analysis if only odds ratio was provided: RR=OR/((1-Pref)+(Pref × OR). In this formula, Pref was the prevalence of the outcome (nephrotoxicity) in the reference non-exposed group. If only the principal data were testified, we converted it into RR value, and calculated the CIs and Pvalues [7]
Some studies provided sample means, SE, and sample size only. Those statistical parameters were enough to calculate the underneath; SD, CI, Z score, P values, OR and RR, using statistical programs and equations. Population mean was measured in the form of adjusted mean baseline level of serum creatinine at both CsA and placebo group. Bearing in mind that only RCTs were included in this meta-analysis, Newcastle-Ottawa Scale (NOS) was attained in the quality scale for each involved publication. Newcastle-Ottawa scale is a quality assessment tool using a scale to evaluate the methodological quality for RCTs, case-control studies, systematic reviews, meta-analyses and cohort studies. In this meta-analysis, the assortment, comparability, and acquaintance of each publication were scored and the articles with NOS score more than six stars were well-thought-out as comparatively ‘high quality’. Any conflicts regarding quality scale, data extraction and data restructuring, were resolved by conversation with the third critic (HHA) [8-10].
Statistical analysis
Bearing in mind the interventional design nature of the encompassed researches, we used for quantitative synthesis a variance components model. As all the involved publications were randomized control trials, OR values were used to assess the correlations between CsA and the risk of nephrotoxicity.
We used both I2 and × 2 statistical tests to carry out the test of heterogeneousness in quantitative calculation through studies. Because tests for heterogeneousness are lacking power, we showed substantial heterogeneousness by considering an I2 value of more than 50% or P value of less than 0.1 in x2 statistic. In this current study, subgroup analyses by stratification of the study characteristics, (such as study site, follow up after withdrawal, potassium, GFR and blood pressure) were steered to identify the sources of heterogeneousness. Impending publication bias would be perceived by both the Egger test and funnel plot analysis. STATA Version 12 (“Stata-corp” stata statistical software: release 12.0, college station, TX) was deployed to perform all the statistical test analyses.
Results
Literature search
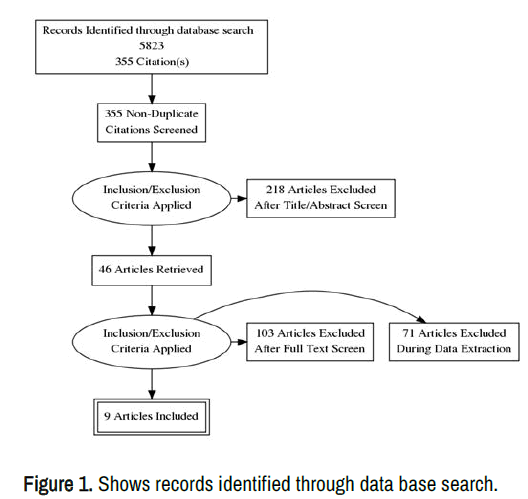
A total of 5823 publications were spotted from the declared databases (1131 in PubMed, 2319 in EMBASE, 512 in web of science and 1539 from the rest of sources). Besides, 322 supplementary records were distinguished through revising the reference lists of pertinent articles. After we excluded 5468 articles with disparate topics, the abstracts of 355 publications were appraised for potential criteria of inclusion [11]. Of the 355 outstanding articles, 218 publications were excluded because they were case reports, narrative reviews and overlaid articles. Besides, the publications in which nephrotoxicity was not involved in the theme, were also dropped out through abstract reviewing. After investigating the full text of the 137 remaining articles, 46 articles were newly added to be involved in the ultimate quantitative synthesis. After the inclusion and exclusion criteria were applied, a total of 103 articles were dropped out after full text investigation and 71 articles excluded also throughout data extraction. However, among the 392 excluded publications, 44 studies didn’t describe the study design clearly, 166 publications didn’t mention the outcome of interest along with data and 4 studies were also excluded because they were prospective cohort studies [12]. In total, 9 publications were published between 1984 and 1999 were included in this study. Our selected nine studies used many variables to assess renal function not only serum creatinine. Two studies of the nine data points, fulfilled all the inclusion criteria and addressed the issue precisely. They were far away from any criteria favors exclusion.
Those two studies used glomerular filtration rate, potassium, renal plasma flow, lithium clearance, blood pressure, plasma albumin and serum bicarbonate as parameters to evaluate the renal function and the degree of nephrotoxicity left behind CsA, rather than serum creatinine. However, it was not in our will to exclude those two RCTs from our study. We just exclude them from the meta-analysis and mention their other findings in the spreadsheet and results. Because this will support our hypothesis. The PRISMA flow diagram for the literature search identifying the relevant studies was present in Figure 1 [13].
Study characteristics
In the seven included studies in this current meta-analysis, a total of 647 participants were involved. The seven studies were published between 1986 and 1999. When the diabetes type was well-thoughtout, only type 1 diabetes mellitus was comprised in the analysis. Among all the studies, the follow-up duration ranged from 6 months to 6 years. The countries where the researches had been conducted were as follows: 2 in Canada, 3 in France, 2 in Denmark (excluded) 1 in Germany and 1 in USA. We assessed the quality of methodology of every included research was by NOS. Newcastle-Ottawa scale, was deliberated as a tool used for assessment of the quality of nonrandomized studies and the full mark was 9 stars. The NOS measures for all the comprised articles ranged from 6 to 9 and the mean score was 7.25 stars. The score is said to be accepted as highquality, is to be more than 6 stars. And this was present in all comprised studies (7 in 9). The foremost characteristics of all the comprised articles in this current study were demonstrated in Table 1 [14].
| Subgroup analysis | Subgroups | No. of studies | Summary effect RR (95% CI) | P value | Study heterogeneity | |
|---|---|---|---|---|---|---|
| I2 (%) | P value | |||||
| Site | France | 3 | 1.40 (1.05-1.87) | 0.65 | 67.6 | 0.218 |
| Canada | 2 | 1.02 (1.014-1.427) | 0.385 | 59.6 | 0.003 | |
| USA | 1 | 1.01 (1.036-1.439) | 0.017 | 33.8 | 0.17 | |
| Germany | 1 | 1.08 (0.670-2.107) | 0.556 | 78.4 | 0.001 | |
| Follow up after withdrawal | Yes | 2 | 1.15 (0.89-1.48) | 0.187 | 32.5 | 0.003 |
| No | 7 | 1.05 (0.48-1.09) | 0.942 | 21.8 | 0.693 | |
| Potassium | Yes | 4 | 1.374 (0.894-2.11) | 0.147 | 33.5 | 0.004 |
| No | 5 | 1.05 (0.46-1.035) | 0.131 | 66.9 | 0.002 | |
| GFR | Yes | 2 | 1.287 (0.934-1.77) | 0.122 | 67.1 | 0.003 |
| No | 7 | 1.066 (0.898-1.26) | 0.462 | 11.7 | 0.34 | |
| Blood pressure | Yes | 2 | 1.276 (0.923-1.76) | 0.141 | 68 | 0.003 |
| No | 7 | 1.073 (0.983-1.39) | 0.076 | 48.2 | 0.102 | |
Note: CI=Confidence Interval, GFR=Glomerular Filtration Rate
Table 1. Summary Relative Risk (RR) and 95% Confidence Interval (CI) for subgroup meta-analysis by study designs and adjusting status.
CsA and risk of nephrotoxicity
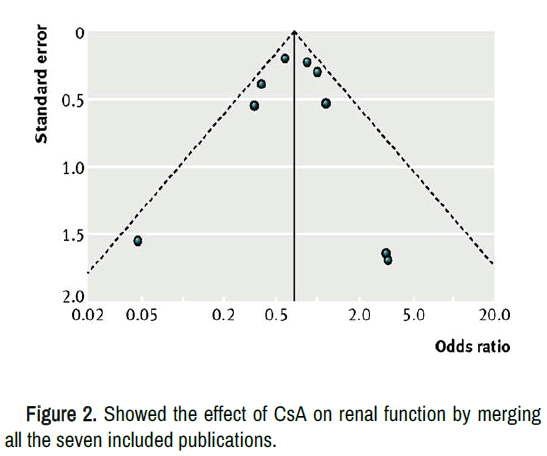
Figure 2 showed the effect of CsA on renal function by merging all the seven included publications in this meta-analysis. The analyses of the seven studies, as a whole, significantly showed that low dose CsA treatment for 12 months was associated with no change or very slight increase in serum creatinine level (OR, 1.06; 95% CI, 1.00-1.43; I 2=73.1%).
To make the conception of the relationship between CsA and nephrotoxicity more deep, among patients treated by CsA and those received placebos or other control groups. A subgroup analyses by status adjustment and study characteristics were steered. When duration analysis of CsA treatment and creatinine level after CsA withdrawal were considered, no significant association between CsA and elevated serum creatinine was detected (RR, 1.15; 95% CI, 0.89-1.48; I2=32.5%) and (RR, 1.05; 95% CI, 0.48-1.09; I2=21.8%) respectively [15]. Subgroup analysis by study locations showed that one study out of three, done in France demonstrated significant relationship between CsA and elevated serum creatinine (RR, 1.40; 95% CI, 1.05-1.87; I2=67.6%) However, none of the studies conducted in Canada, USA or Germany demonstrated statistically significant association. (RR, 1.02; 95% CI, 1.014-1.427; I2=59.6%), (RR, 1.01; 95% CI, 1.036-1.439; I2=33.8%), and (RR, 1.08; 95% CI, 0.670-2.107; I2=78.4%) respectively. Upon subgroup analysis by GFR, serum potassium, and blood pressure no significant association between CsA and affection of those parameters was detected. When the adjustment status was considered and no significant association was detected in subgroup meta-analysis by the adjustments of mentioned parameters.
Sensitivity analysis and publication bias
To evaluate the strength of the conclusion in this research, we steered a sensitivity analysis via exclusion of the articles with low quality of methodology (less than six stars in NOS). We did not drop out any article from the sensitivity analysis to ensure balanced assessment of the statistical relationship between CsA as a significant harmful factor elevating serum creatinine level. After excluding 1 study from the meta-analysis, it was found that the net results favors absence of CsA associated nephrotoxicity with no significant harmful effect for kidney (RR, 1.22; 95% CI, 1.00-1.47; I2=62.9%). To evaluate the publication bias, we used both Egger test and visual scrutiny of funnel plots. No momentous publication bias was noticed in the designated 9 studies (eegg test, P=0.380; begg test, P=0.190) [16].
Discussion
This meta-analysis-of seven randomized control trials on CsA for nephrotoxicity risk-do not deny the absence of a degree of harm, however, it demonstrated the absence of a significant harmful effect for incidence of permanent nephrotoxicity. Nephrotoxicity was insignificant and transient, compared to the benefit of CsA in remission of newly onset juvenile diabetes, with preservation of beta cell function through the first year followed the diagnosis [17]. In general the conclusion was hearty and no publication bias was sensed. However, forward-looking progressive analyses by status adjustments and study designs showed no significant correlations, also, showed absence of intolerable, significant or permanent side effects. And this was clear in the effect of CsA on GFR, serum potassium, renal plasma flow, lithium clearance, serum albumin and bicarbonate, 6 months after withdrawal and even during the course of treatment. Not to mention the sub-group analysis by study sites, GFR, serum potassium, follow up after withdrawal and blood pressure. Prolonged treatment of high dose CsA, which was a major participator in treatment of many autoimmune diseases and in the field of transplantation, was reported to be associated with development of many side effects [18].
CsA, the aforementioned, was used in treatment of new onset type 1 juvenile diabetes. It Causes remission and autoimmune suppression of antibodies. Therefore, restoration of beta cell function and patients protection from final adverse undesirable outcome, reducing by that morbidity and mortality. However, it may lead to transitional outcomes as a drawback of CsA itself. These adverse effects were proved by researches, to be minor and transient, where the creatinine level did not exceed 160 umol/L. The clinical and biochemical side effects of cyclosporine came across this meta-analysis were not greater than expected.
The level of serum creatinine in all studies selected was established by six months and lingered stable through the first year. When we compared the estimation of Glomerular Filtration Rate (GFR) made in the same subjects, in the selected studies used in subgroup analysis, we accepted our alternative hypothesis. As shown in a study done on 49 subjects on cyclosporine and 45 subjects on placebo, which indicated alike equivalent reductions of both renal functions in cyclosporine-treated subjects (serum creatinine 18%, GFR 20%) [19].
Feldt and his colleagues did not use the creatinine as indicator for renal function evaluation, however, the renal function in terms of creatinine clearance was returned to normal following withdrawal of CsA. It was noticed that reduction in GFR, renal plasma flow and lithium clearance, had disappeared, six months after withdrawal of CsA. The net result of our analysis demonstrated absence of serious nephrotoxicity that could be observed. In all studies reviewed, the rise in plasma creatinine above normal in cyclosporine treated subjects was transient and insignificant.
The difference noticed between the uppermost levels in serum creatinine level when we come to compare it with the placebo group was insignificant. However in most of studies when the dose of CsA was remodeled, all the parameters used to evaluate the kidney functions was normalized and improved within less than six months. No one could deny the presence of minor adverse effects in order to obtain the desired effect of the drug, among the subjects of the study population treated with CsA. However, none of the researchers was obliged to suspend the treatment. Additionally, the double-blind nature of the trials might have a trivial effect, if any, which testifies the occurrence of such similar side effects in the placebo group. The reversible increase in serum creatinine was the gravest side effect noticed in most of the included and excluded trials, even the one which disturb the balance of our meta-analysis. Secondary side effects and drawbacks of CsA administration at low to moderate doses were infrequent and negligible. Serum level of creatinine did not change considerably in the study group treated with cyclosporine [20].
Trials conducted on cyclosporine have demarcated a structure of cause and effect that passes from augmentation of endogenous insulin release by immunotherapy to glycemic control to decrease in peripheral neuropathy diabetic retinopathy and microvascular pathology. We imagine that further clinical trials will keep an eye on these visions and we hope that this hard work will lead to a foremost bargain in the disease’s burden of grief. The limitation of the study was, some of the available data was abundant but descriptive and confined to; numbers, means, SEs and p values, with no further statistical analysis. This put a heavy load over us and pushed us for more digging and in-depth searching and analysis. For example the author mentioned in the last paragraph that p value was considered to be <0.05, we extract the rest of data by ourselves like mean differences, differences between groups, upper level and lower level CIs.
Conclusion
On 1984 Canadian endocrinologists tried to examine the effect of low-dose, short term CsA for patients, newly diagnosed with type one diabetes mellitus, for remission and restoration of the beta cell function, think of them, it will suppress the fierceness of the autoimmune attack against islets of Langerhans. This topic was addressed extensively from 1984 till 1999, and no scholars thought to knock the door again. Although the conclusions of most of the articles were vague and neutral, most of the clinicians, till now insist to put CsA in the dock. It was an arbitrary verdict. We conducted this first meta-analysis to put points on the letters and cut doubt in certainty, that low-dose, short term CsA has no effect on this kidney, and if so it is trivial and reversible.
Acknowledgment
We would like to thank Asem Ahmad, RN PhD and Nahla Naser MD PhD for their review.
Conflict of Interest
The authors certify that they have no conflicts of interest to declare including but not limited to financial, consultancy, advisory, institutional and other relationships that might lead to a possible bias or misconstrue the results and/or conclusions of this research. PRISMA 2009 Checklist statement: The authors certify that the guidelines of the PRISMA 2009 statement have been adopted.
Authors Contribution
AME, AAE, SAA and HHA, contributed in the design, analysis and elucidation of the results and conscripted the manuscript. HHA, SAA steered the preliminary literature search. AAE and AME conducted the appraisal of the literature and included publications according to the aptness and accomplished the data collection. All the authors revised the manuscript and approved the final version.
References
- Colombo, Maria Delia, Renata Perego and Gilberto Bellia. "Cyclosporine-Associated Nephrotoxicity." Open J Nephrol 3 (2013): 168-169.
- Kahan, BD "Cyclosporine Nephrotoxicity: Pathogenesis, Prophylaxis, Therapy, and Prognosis." Am J Kidney Dis 8 (1986): 323-331.
[Crossref] [Google Scholar] [PubMed]
- Paller, Mark S. "Cyclosporine Nephrotoxicity and the Role of Cyclosporine in Living-Related Donor Transplantation." Am J Kidney Dis 16 (1990): 414-416.
[Crossref] [Google Scholar] [PubMed]
- Ribstein, Jean, Michel Rodier and Albert Mimran. "Effect of Cyclosporine on Blood Pressure and Renal Function of Recent Type 1 Diabetes Mellitus." J Hypertens Suppl 7 (1989): 198-199.
[Crossref] [Google Scholar] [PubMed]
- Best, Nicola G, Andrew K Trull, Keith KC Tan and David J Spiegelhalter, et al. "pharmacodynamics of Cyclosporine in Heart and Heart-Lung Transplant Recipients: I: Blood Cyclosporine Concentrations and Other Risk Factors for Cardiac Allograft Rejection. Transplantation 62 (1996): 1429-1435.
[Crossref] [Google Scholar] [PubMed]
- Yocum, David E. "Cyclosporine in Rheumatoid Arthritis: Beyond Experimentation." Semin Arthritis Rheum 1992.
[Google Scholar] [PubMed]
- Montano, AJS, Wasilenko J Bintner AL Mason "Cyclosporine a Protects Against Primary Biliary Cirrhosis Recurrence After Liver Transplantation." Am J Transplant 10 (2010): 852-858.
[Crossref] [Google Scholar] [PubMed]
- Rocha, Guillermo, Jean Deschenes Marcelo Cantarovich. "Cyclosporine Monitoring With Levels 6 Hours after the Morning Dose in Patients with Noninfectious Uveitis." Ophthalmology 104 (1997): 245-251.
[Crossref] [Google Scholar] [PubMed]
- Myers, Bryan D, Richard Sibley, Lynne Newton and Stephen J. et al. "The Long-Term Course Of Cyclosporine-Associated Chronic Nephropathy." Kidney Int 33 (1988): 590-600.
[Crossref] [Google Scholar] [PubMed]
- Assan, R, M Debray-Sachs, C Laborie and L Chatenoud, et al. "Metabolic and Immunological Effects of Cyclosporin in Recently Diagnosed Type 1 Diabetes Mellitus." The Lancet 325 (1985): 67-71.
[Crossref] [Google Scholar] [PubMed]
- Assan, Roger, Francoise Blanchet, Gilles Feutren and Jose Timsit, et al. "Normal Renal function 8 to 13 years after Cyclosporin a Therapy in 285 Diabetic Patients." Diabetes Metab Res Rev 18 (2002): 464-472.
[Crossref] [Google Scholar] [PubMed]
- Moher, David, Larissa Shamseer, Mike Clarke and Davina Ghersi, et al. "Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015 Statement." Syst Rev 4 (2015): 1-9.
- Stroup, Donna F, Jesse A Berlin, Sally C Morton and Ingram Olkin, et al. "Meta-Analysis of Observational Studies in Epidemiology: A proposal for Reporting." Jama 283 (2000): 2008-2012.
- Conn, Vicki S, Todd M Ruppar, Lorraine J Phillips and Jo-Ana D Chase "Using Meta-Analyses for Comparative Effectiveness Research." Nurs Outlook 60 (2012): 82-190.
[Crossref] [Google Scholar] [PubMed]
- Matz, Robert. "Cockcroft-Gault Equation and Estimation of Creatinine Clearance." Am J Med 112 (2002): 684-685.
[Crossref] [Google Scholar] [PubMed]
- Melsen, WGMCJ, Bootsma MM and Rovers MJM Bonten "The Effects of Clinical and Statistical Heterogeneity on the Predictive values of Results from Meta-Analyses." Clin Microbiol Infect 20 (2014): 123-129.
[Crossref] [Google Scholar] [PubMed]
- Song, Jae W Kevin C Chung "Observational Studies: Cohort and Case-Control Studies." Plast Reconstr Surg 126 (2010): 2233-2234.
[Crossref] [Google Scholar] [PubMed]
- Grimes, David A and Kenneth F Schulz. "Making Sense of Odds and Odds ratios." Obstet Gynecol 111 (2008): 423-426.
[Crossref] [Google Scholar] [PubMed]
- Greenland, Sander, Stephen J Senn, Kenneth J Rothman and John B Carlin, et al. "Statistical Tests, P values, Confidence Intervals, and Power: A guide to Misinterpretations." Eur J Epidemiol 31 (2016): 337-350.
- Barde, Mohini P and Prajakt J Barde. "What to Use to Express the Variability of Data: Standard Deviation or Standard Error of Mean?" Perspect Clin Res 3 (2012): 112-113.
[Crossref] [Google Scholar] [PubMed]
Author Info
1Department of Public Health and Community Medicine, King Saud University, Riyadh, Saudi ArabiaDepartment of Medicine, University of Washington, Washington, United States
Received: 19-Aug-2019, Manuscript No. JDCM-23-103309; Editor assigned: 22-Aug-2019, Pre QC No. JDCM-23-103309 (PQ); Reviewed: 05-Sep-2019, QC No. JDCM-23-103309; Revised: 30-Jun-2023, Rev Manuscript No. JDCM-23-103309 (R); Published: 28-Jul-2023, DOI: 10.37421/2475-3211.2023.8.205, QI NUMBER: JDCM-23-103309
Citation: El-Malky Ahmed M and Ramachandra G Naik. "Cyclosporine Nephrotoxicity in Patients with Type 1 Diabetes Mellitus Arbitrary Verdict: A Meta-Analysis of Randomized Control Trials ." J Diabetic Complications Med 8 (2023): 205.
Copyright: © 2023 El-Malky AM, et al. This is an open-access article distributed under the terms of the creative commons attribution license which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.