Research Article - (2022) Volume 13, Issue 5
Received: 27-Jun-2022, Manuscript No. jbmbs-22-67765;
Editor assigned: 29-Jun-2022, Pre QC No. P-67765;
Reviewed: 11-Jul-2022, QC No. Q-67765;
Revised: 15-Jul-2022, Manuscript No. R-67765;
Published:
22-Jul-2022
, DOI: 10.37421/2155-6180.2022.13.110
Citation: Adjei, Augustine Kena, Pascal Kingsley Kataboh, Faustina Asante and Enoch Boyetey. “A Binary Logistic Regression Analysis on the Factors Associated with High Blood Pressure and its Related Heart Issues.” J Biom Biostat 13 (2022): 110.
Copyright: © 2022 Adjei AK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Hypertension is a major public health issue and an important research topic because of its great incidence and role as a key risk factor for cardiovascular disease and other consequences. The goal of this study is to determine the association between gender and blood pressure, as well as to determine which race suffers the most from high blood pressure among study participants. It may be concluded from the findings of this study that elderly persons have a larger risk of high blood pressure than younger people. High blood pressure is also more common in African Americans (AA) than in other races. Women are more likely than men to have high blood pressure, and smokers are more likely than non-smokers to have high blood pressure. Physical activity aids in the burning of calories, which aids in weight loss. As a result, thick and hefty persons have a larger risk of high blood pressure than small people. Obesity and advancing age have been shown to be independent risk factors for high blood pressure. Improvements to surveillance systems are required, as is the introduction of community-based screening programs for the early detection of high blood pressure. Because there was a lack of understanding of high blood pressure among high blood pressure patients, improving health literacy to raise awareness of high blood pressure is also a pressing necessity. Weight control improved physical activity, increased fruit and vegetable consumption, and smoking ban are all essential and suggested interventions.
Blood pressure • Cardiovascular diseases • Hypertension • Obesity
Cardiovascular diseases (CVDs) are the major cause of death, claiming the lives of an estimated 17.9 million people per year. CVDs are a set of heart and blood vessel disorders that comprise coronary heart disease, cerebrovascular disease, rheumatic heart disease, and other conditions [1]. Heart attacks and strokes account for more than four out of every five CVD deaths, with one-third of these deaths occurring before the age of 70 [2]. Unhealthy food, physical inactivity, cigarette use, and excessive alcohol consumption are the major behavioral risk factors for heart disease and stroke [3]. Individuals may experience symptoms such as high blood pressure, high blood glucose, high blood lipids, and overweight or obesity as a result of behavioral risk factors. These intermediate-risk factors can be assessed in primary healthcare settings and suggest a higher risk of heart attack, stroke, heart failure, and other consequences [4]. Tobacco cessation, salt reduction in the diet, increased fruit and vegetable consumption, regular physical activity, and avoidance of problematic alcohol use have all been demonstrated to lessen the risk of cardiovascular disease. Health policies that foster conditions that make healthy options affordable and accessible are critical for encouraging people to develop and maintain healthy habits [5].
Heart disease is caused by high blood pressure, which is a key risk factor. It is a medical disorder in which the blood pressure in your arteries and other blood vessels becomes excessively high. To lessen your risk of heart disease and heart stroke, you can lower your blood pressure with lifestyle modifications or medication [6]. High blood pressure, heart disease, and other related disorders are likely to be influenced by genetic factors. People with a family history of heart disease are more likely to share shared settings and other factors that may enhance their risk [7]. Cholesterol is a waxy, fat-like substance produced by the liver and contained in several foods. Extra cholesterol can build up in the walls of arteries, especially those of the heart, if we consume more cholesterol than our bodies can use. The arteries narrow as a result, reducing blood flow to the heart, brain, kidneys, and other organs of the body. There are frequently no signs or symptoms of high blood cholesterol [8]. For energy, your body needs glucose (sugar). Insulin is a hormone produced by the pancreas that aids in the transport of glucose from your diet to your body's cells for energy. If you have diabetes, your body either doesn't create enough insulin or can't use it properly, or both. Sugar builds up in the bloodstream as a result of diabetes [9]. Obesity is defined as having too much bodily fat. Obesity has been linked to high blood pressure, diabetes, and heart disease. Smoking raises your chances of developing heart disease and having a heart attack. Cigarette smoking can harm your heart and blood arteries, increasing your risk of cardiac problems such as atherosclerosis and heart attacks [10]. Identification of risk factors is a must before effective prevention strategies can be implemented. The goal of this research is to learn more about the factors that contribute to high blood pressure and the heart problems that come with it.
Objectives of the study
The objectives of this study were:
I. To investigate the relationship between gender and blood pressure.
II. To determine the races that suffered most as a result of high blood pressure.
III. To determine whether high blood pressure was caused by obesity.
IV. To investigate whether smoking affected blood pressure.
Research questions
Our research aimed to address the following questions:
1. What is the relationship between gender and blood pressure?
2. Which races suffer as a result of high blood pressure?
3. Is high blood pressure caused by obesity?
4. Does smoking affect blood pressure?
Literature review research
Cardiovascular diseases (CVDs) are the most common cause of death around the world. CVDs claimed the lives of 17.9 million individuals worldwide in 2019, accounting for 32% of all deaths. Heart attacks and strokes were responsible for 85 percent of these deaths [1]. Low- and middle-income countries account for more than three-quarters of CVD mortality [11]. CVDs were responsible for 38% of the 17 million premature deaths (before the age of 70) related to non communicable diseases in 2019 [1]. Most cardiovascular illnesses can be avoided by addressing behavioral risk factors such as cigarette use, poor diet and obesity, physical inactivity, and problematic alcohol consumption. It is critical to recognize cardiovascular illness as soon as feasible in order to initiate treatment with counseling and medications [5].
Cardiovascular diseases (CVDs) are a group of disorders of the heart and blood vessels. They include:
Coronary heart disease is a condition that affects the blood arteries that nourish the heart muscle.
• Cerebrovascular disease (CVD) is a condition that affects the brain's blood arteries.
• Peripheral arterial disease (PAD) is a condition that affects the blood arteries that deliver blood to the arms and legs.
• Rheumatic heart disease - rheumatic fever, which is caused by streptococcal bacteria, damages the heart muscle and heart valves.
• Congenital heart disease - birth abnormalities that disrupt the heart's normal development and function as a result of malformations in its structure from birth; and
• Pulmonary embolism and deep vein thrombosis - blood clots in leg veins that might dislodge and go to the heart and lungs.
Heart attacks and strokes are frequently sudden occurrences caused by a blockage that prevents blood from reaching the heart or the brain. A build-up of fatty deposits on the inner walls of the blood arteries that supply the heart or brain is the most common cause [6]. Strokes are caused by blood clots or bleeding from a blood artery in the brain. Unhealthy food, physical inactivity, cigarette use, and problematic alcohol consumption are the most major behavioral risk factors for heart disease and stroke [2]. Raised blood pressure, raised blood glucose, raised blood lipids, and overweight or obesity are all symptoms of behavioral risk factors [10]. CVDs are also influenced by several underlying factors. Globalization, urbanization, and population ageing are the key drivers driving social, economic, and cultural change. Poverty, stress, and genetic factors are also predictors of CVDs [7]. Furthermore, pharmacological treatment for hypertension, diabetes, and high blood lipids is required to lower cardiovascular risk and prevent heart attacks and strokes in persons who have these illnesses [5]. Low- and middle-income nations account for at least three-quarters of all CVD deaths worldwide. People in low- and middle-income countries frequently lack access to basic health care services that allow for early detection and treatment of people with CVD risk factors. People with CVDs and other non-communicable illnesses in low- and middle-income countries have reduced access to effective and equitable health care services that meet their needs. As a result, in many of these nations, disease identification occurs late in the course of the disease, and people die of CVDs and other noncommunicable diseases at a younger age, often during their most productive years. The poorest individuals in low- and middle-income countries are the ones who bear the brunt of the consequences. Evidence is accumulating that CVDs and other non-communicable illnesses lead to poverty at the household level due to catastrophic health spending and high out-of-pocket expenses. CVDs impose a significant economic burden on the economies of low- and middle-income countries [11]. Women and men's cholesterol levels rise as they age. Women have lower total cholesterol levels than men of the same age before menopause. Women's cholesterol levels tend to climb after they reach menopause.
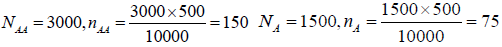
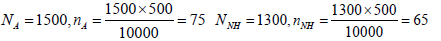
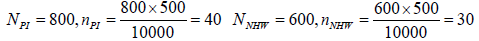
Sampling technique
A stratified sampling technique was used to get the respondents for the study, which was conducted in Birmingham. This sampling technique was chosen because we wanted to divide the population into smaller groups that do not overlap. This is because we wanted to consider respondents from different races: African American (AA), American Indian (AI), Native Hawaiian (NH), Pacific Islander (PI), and Non-Hispanic White (NHW). In that case, every race would be studied thoroughly and explicitly [12].
Formula for getting a sample size using stratified sampling technique
The objective of stratification was to produce estimators of sample sizes for each stratum (different races) such that with each stratum, the units are as similar as possible. The stratification was based on the different races in the United States of America.

Where is the total sample size, is the population size, is the size of the stratum, and is the size of the sample selected from the stratum. The five different strata are AA, AI, NH, PI, and NHW.
N =10000, n = 500
Research design
An appropriate research design was needed to strategize how respondents would answer the research questions. In that regard, descriptive and correlational designs were used to allow us to measure variables and describe relationships between them. These well-planned research designs helped ensure that the method matched the research aims and objectives [13-18].
Data analysis
Descriptive statistics: An appropriate marginal plot is used to assess the relationship between the weight and age of respondents. It examines the distributions of weight and age. The marginal plot indicates that the data has no outliers. Thus no other extraneous factors affect the data [19]. Since the data points in the marginal plot are scattered randomly, it implies that there is no relationship or correlation between weight and age. Thus, weight cannot predict age and vice versa. Thus, older people are not heavier than younger people and vice versa (Figure 1).
People and vice versa from the line plot of the mean (AGE), generally, it was observed that older people had higher blood pressure than young people [20-24]. Thus, older people are at a higher risk of having high blood pressure as compared to young people. High blood pressure is more prevalent among African Americans (AA) than among the other races (Figure 2).
From the line plot of the mean (WEIGHT), generally, it was observed that thick and heavy people (obese) had higher blood pressure than slim people. Engaging in physical exercise would help burn calories which in turn help reduce weight. Thus, thick and heavy people are at a higher risk of having high blood pressure as compared to slim people (Figure 3).
Table 1 was used to determine whether the association between high blood pressure and each of the predictor variables is statistically significant. From Table 2 (p-value), age, weight, and smoking habits are statistically significant. Sex and race are not statistically significant [25]. This means that whereas age, weight, and smoking habits contribute to the prediction of blood pressure, race and sex do not contribute to the prediction of blood pressure.
| Variables | Value | Count |
|---|---|---|
| Blood Pressure Systolic/Diastol | N | 142 (Event) |
| H | 358 | |
| Total | 500 |
| Term | Coef | SE Coef | Z-Value | P-Value | VIF |
|---|---|---|---|---|---|
| Constant | 27.77 | 3.35 | 8.28 | 0.000 | |
| Age | -0.05212 | 0.00893 | -5.84 | 0.000 | 1.29 |
| Weight (Pounds) | -0.1138 | 0.0149 | -7.61 | 0.000 | 1.34 |
| Race | |||||
| AA | -0.220 | 0.465 | -0.47 | 0.636 | 2.10 |
| AI | -0.036 | 0.466 | -0.08 | 0.939 | 2.03 |
| NH | -0.439 | 0.536 | -0.82 | 0.413 | 1.65 |
| NHW | -0.526 | 0.689 | -0.76 | 0.445 | 1.37 |
| PI | -0.152 | 0.625 | -0.24 | 0.808 | 1.43 |
| Sex | |||||
| W | -0.058 | 0.295 | -0.20 | 0.844 | 1.03 |
| Smoking | |||||
| Y | -3.676 | 0.366 | -10.05 | 0.000 | 1.51 |
Negative coefficients indicate that the event becomes less likely as the predictor increases whereas positive coefficients indicate that the event becomes more likely as the predictor increases. From Table 3, the coefficients of age, weight, and smoking suggest that higher age, weight (obesity), and excessive smoking are associated with lower probabilities that the event (Normal blood pressure) will occur.
| Wald Test | |||
|---|---|---|---|
| Source | DF | Chi-Square | P-Value |
| Regression | 9 | 117.03 | 0.000 |
| Age | 1 | 34.06 | 0.000 |
| Weight (Pounds) | 1 | 57.99 | 0.000 |
| Race | 5 | 1.28 | 0.937 |
| Sex | 1 | 0.04 | 0.844 |
| Smoking | 1 | 101.07 | 0.000 |
From the ANOVA, Table 4, the logistic regression model is statistically significant. Even though the overall regression model is statistically significant, some of the predictor variables (race, sex) are not statistically significant.
| Variables | Odds Ratio | 95% CI |
|---|---|---|
| Age | 0.9492 | (0.9327, 0.9660) |
| Weight (Pounds) | 0.8924 | (0.8666, 0.9189) |
Odds ratios that are greater than 1 indicate that the event is more likely to occur as the predictor increases. Since the odds ratios are less than 1 for both age and weight, we conclude that the event (Normal blood pressure) is less likely to occur as age and weight increase [26]. Thus, high blood pressure occurs as a result of old age and obesity.
The odds ratio for level-A relative to level-B
Odds ratios for categorical predictors: For categorical predictors, if the odds ratio is less than 1, then it implies that the event (Normal blood pressure) is less likely to occur at level A. On the contrary, if the odds ratio is greater than 1, then it implies that the event (Normal blood pressure) is more likely to occur at level A [27].
Race: From the Table 5, Normal blood pressure is less likely to occur at AA than at A. Thus, AA is more likely to have a high blood pressure than A. Normal blood pressure is less likely to occur at AI than at A. Thus, AI is more likely to have a high blood pressure than A. Similarly, Normal blood pressure is less likely to occur at NH, NHW, and PI than at A. Thus, NH, NHW, and PI are more likely to have a high blood pressure than A [28].
| Level A | Level B | Odds Ratio | 95% CI |
|---|---|---|---|
| Race | |||
| AA | A | 0.8027 | (0.3229, 1.9955) |
| AI | A | 0.9651 | (0.3870, 2.4069) |
| NH | A | 0.6450 | (0.2258, 1.8426) |
| NHW | A | 0.5910 | (0.1531, 2.2815) |
| PI | A | 0.8593 | (0.2527, 2.9226) |
| AI | AA | 1.2022 | (0.5491, 2.6324) |
| NH | AA | 0.8035 | (0.3156, 2.0453) |
| NHW | AA | 0.7362 | (0.2089, 2.5947) |
| PI | AA | 1.0705 | (0.3484, 3.2890) |
| NH | AI | 0.6683 | (0.2598, 1.7194) |
| NHW | AI | 0.6124 | (0.1697, 2.2094) |
| PI | AI | 0.8904 | (0.2875, 2.7572) |
| NHW | NH | 0.9163 | (0.2345, 3.5803) |
| PI | NH | 1.3323 | (0.3843, 4.6188) |
| PI | NHW | 1.4540 | (0.3234, 6.5380) |
| Sex | |||
| W | M | 0.9436 | (0.5297, 1.6807) |
| Smoking | |||
| Y | N | 0.0253 | (0.0124, 0.0518) |
From the Table 5, Normal blood pressure is less likely to occur at AI and PI than at AA whereas Normal blood pressure is more likely to occur at NH and NHW than at AA. Thus, AI and PI are more likely to have a high blood pressure than AA while NH and NHW are more likely to have Normal blood pressure than AA.
Again, Normal blood pressure is less likely to occur at NH, NHW, and PI than at AI. Thus, NH, NHW, and PI are more likely to have a high blood pressure than AI.
Normal blood pressure is less likely to occur at NHW than at NH whereas Normal blood pressure is more likely to occur at PI than at NH. Thus, NHW are more likely to have a high blood pressure than NH while PI are less likely to have a high blood pressure than NH [29].
Normal blood pressure is more likely to occur at PI than at NHW. Thus, PI is less likely to have high blood pressure than NHW.
Sex: Women are less likely to have a normal blood pressure than men. Thus, women tend to have a high blood pressure than men.
Smoking: People who smoke are more likely to have a high blood pressure than those who do not smoke. This implies that smoking tends to affect heart conditions.
Deviance R-sq, Deviance R-sq(adj) and AIC
To determine how well the model fits the data, examine the statistics in the Model Summary (Table 6). The data format affects the deviance statistics but not the AIC. The higher the deviance, the better the model fits the data. The smaller the AIC, the better the model fits the data.
| Deviance R-Sq |
Deviance R-Sq(adj) |
AIC | AICc | BIC | Area Under ROC Curve |
|---|---|---|---|---|---|
| 87.15% | 84.64% | 23.45 | 23.90 | 65.59 | 0.7284 |
In these results, the model explains 87.15% of the deviance in the response variable. The deviance value indicates that the model provides a good fit to the data. Similarly, a high adjusted deviance value and a small AIC value indicate that the model fits the data well.
Goodness of fit test
The goodness-of-fit-test is used to determine whether the predicted probabilities deviate from the observed probabilities in a way that the binomial distribution does not predict. If the p-value for the goodness-of-fit test is lower than the significance level of 0.05, then the predicted probabilities deviate from the observed probabilities in a way that the binomial distribution does not predict. If the p-value is less than 0.05, then the deviation is statistically significant and thus a different link functions or change the terms in the model.
For binary logistic regression, the format of the data affects the p-value because it changes the number of trials per row.
In these results, the goodness-of-fit-tests p-values are greater than the significance level of 0.05, which indicates that there is not enough evidence to conclude that the model does not fit the data (Table 7).
| Test | DF | Chi-Square | P-Value |
|---|---|---|---|
| Deviance | 490 | 303.45 | 0.549 |
| Pearson | 490 | 397.18 | 0.848 |
| Hosmer-Lemeshow | 8 | 6.92 | 0.446 |
It may be concluded from the findings of this study that elderly persons have a larger risk of high blood pressure than younger people. High blood pressure is also more common in African Americans (AA) than in other races. Women are more likely than men to have high blood pressure, and smokers are more likely than nonsmokers to have high blood pressure. Physical activity aids in the burning of calories, which aids in weight loss. As a result, thick and hefty persons have a larger risk of high blood pressure than small people. Obesity and increasing age have been shown to be independent risk factors for high blood pressure. Improvements to surveillance systems are required, as is the introduction of community-based screening programs for the early detection of high blood pressure. Because there was a lack of understanding of high blood pressure among high blood pressure patients, improving health literacy to raise awareness of high blood pressure is also a pressing necessity. Weight control improved physical activity, increased fruit and vegetable consumption, and smoking ban are all essential and suggested interventions.
The following are some of the study's limitations:
1. The study was only conducted in an urban area.
2. An important risk factor for hypertension is stress. For improved outcomes, it could also be considered in the current investigation.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google ScholarCrossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Journal of Biometrics & Biostatistics received 3496 citations as per Google Scholar report