Review Article - (2023) Volume 8, Issue 5
Received: 18-Feb-2023, Manuscript No. JPNP-23-89636;
Editor assigned: 21-Feb-2023, Pre QC No. JPNP-23-89636 (PQ);
Reviewed: 08-Feb-2023, QC No. JPNP-23-89636;
Revised: 17-May-2023, Manuscript No. JPNP-23-89636 (R);
Published:
25-May-2023
, DOI: 10.37421/2472-0992.2023.9.248
Citation: Daf, Abhijit N, Gauri S Dhandre, Akash S
Kapse and Shailesh B Pise, et al. "A Review on: Synthetic and Herbal
Approaches for the Treatment of Alzheimer’s disease." J Pharmacogn Nat
Prod 9 (2023): 248.
Copyright: © 2023 Daf AN, et al. This is an open-access article distributed under the terms of the creative commons attribution license which permits unrestricted use,
distribution and reproduction in any medium, provided the original author and source are credited.
Alzheimer’s Disease/Disorder (AD) is common kind of neurodegenerative cause of dementia. The treatments available for AD are completely symptoms preventive this Review was done with the objective to analyze and estimate for the herbal and synthetic approaches for the treatment of AD. The article review and analysis has gone through 8-10 herbal drugs and around 10-12 drugs from synthetic sources. The antioxidant potential of herbal drugs is found to be quite effective as that of synthetics. Thus this article proves more potency of herbs in the treatment of AD.
Alzheimer’s Disease (AD) • Pathophysiology • Epidemiology • Diagnosis of AD • Neuropathology • Herbal drugs • Synthetic drugs
Alzheimer's Disease (AD) is the most common cause of dementia and is clinically characterized by a progression from episodic memory problems to a slow general decline of cognitive function [1]. In 2013, ~44 million of the worldwide population was expected to be affected by dementia and a steep rise to ~136 million has been predicted by 2050 [2]. To date, there are no treatments with proven disease modifying effects and AD remains the largest unmet medical need in neurology. AD pathology presents a complex interplay between several biochemical alterations, including changes in amyloid precursor protein metabolism. Phosphorylation of the tau protein oxidative stress, impaired energetics, mitochondrial dysfunction, inflammation, membrane lipid deregulation and neurotransmitter pathway disruption [3]. Most of these pathological features can be directly linked to metabolic abnormalities and it is now clear that metabolic dysfunction is an important factor in AD [4]. For example, impaired cerebral glucose uptake occurs decades prior to the onset of cognitive dysfunction and is an invariant feature of AD [5]. The well documented neurotoxicity associated with Aβ42 is thought to participate in impaired neuronal energetics through initiating a cascade of pathological events; interaction between Aβ42 and mitochondrial enzymes leads to increased release of Reactive Oxygen Species (ROS), affecting glycolysis, the TCA cycle and mitochondrial respiratory chain activity through the accumulation of deleterious intermediate metabolites in the mitochondria [6,7].
Alois Alzheimer and Auguste D
The German psychiatrist and neuropathologist Dr. Alois Alzheimer is credited with describing for the first time a demanding condition which later became known as AD. In his landmark 1906 conference lecture and a subsequent 1907 article, Alzheimer described the case of Auguste D, a 51 years old woman with a ‘peculiar disease of the cerebral cortex,’ who had presented with progressive memory and language impairment, disorientation, behavioral symptoms (hallucinations, delusions, paranoia), and psychosocial impairment [8-10].
Normal memory
In order to understand the complexities of dementia, it is necessary to describe what happens in normal ageing and understanding what can go wrong and gives rise to abnormal conditions such as dementia. Ageing can be distinguished in terms of biological, social and psychological disciplines, but there is often a great overlap and interaction between them. For example, a physical change such as arthritis can limit mobility, which in turn can reduce involvement in social activities or other previous sources of enjoyment [11]. The influence of one aspect of ageing on another should also be remembered; this is important when considering and comparing past and present cognitive functions within the same person defining 'normal' is a difficult task and it is surprising how 'normal' and 'abnormal' activities and attitudes often overlap. The blurring of boundaries occurs between different cultures, different environments or even between individuals. A misconception is to consider normality as distinct and opposite to abnormality when in fact 'normality' refers to the 'range around the middle of a dimension (e.g., height) with two extremes at opposite ends (very tall and very short), rather than one extreme. Different people have their own opinion about normality and hence expectancies in ageing are perceived differently between individuals. With the advance of medicines and technology, people are generally living longer and so more people are exposed to older people and are witness to the variations in ageing of relatives and friends. In turn, people's understanding of normal ageing is being constantly revised and so too are their expectancies of themselves and others. Normal ageing brings with it changes, not just to an individual's appearances, however subtle, but also certain changes to the higher mental functions or 'cognitive' functions [12,13]. Memory can also be affected, sometimes because the individual has failed to receive information correctly or sometimes because it can no longer be effectively encoded or stored. The effect of ageing on memory, particularly episodic memory, is very often one of the first of the cognitive functions to be noticed by others and can cause considerable distress to the individual and to relatives, close friends and careers. Deterioration in memory functioning is characteristic dementia. But it can also indicate other dysfunctions which should always be considered in any assessment.
Memory functioning has been recognized as follows:
Short-term and long-term memory: Short-term memory, now elaborated into the concept of working memory, is the system which allows one to remember a new telephone number while one is dialing it, so long as one is not distracted.
Long-term memory allows one to remember a familiar telephone number from day to day and year to year.
• Semantic and episodic memory: Different types of knowledge
appear to be stored differently. A distinction drawn
initially between episodic and semantic memories and, more
latterly, a contrast between procedural and declarative
memories has gained acceptance. Episodic memories are for
particular events, while semantic memories are context free facts.
• Declarative and procedural memory: Both semantic and
episodic memories may be subsumed under this heading
(which represents the memory for facts). Procedural memory is
for skills and routines and may include some types of sensory
stimuli. For example, knowing how to drive a car is a
procedural memory, knowing how the engine works is
declarative. Generally, older people can learn as much as
younger people, but more time is needed for them to achieve
the same level of learning as they cannot process and 'absorb'
information as quickly as younger people. Sometimes this speed
reduction becomes notice able and marked and may accompany the
onset of depression.
Problems with memory
Memory failure is a common and significant problem in dementia. It is now believed that there are four stages involved in memory: registration, encoding, storage and retrieval. For information to be stored in memory it must first be attended to or registered [14]. Encoding is the process whereby this information may be semantically encoded or phonologically encoded, i.e. encoded in terms of meaning or sound, respectively. Storage is the process by which information is maintained in memory. It is widely accepted that different types of knowledge appear to be stored differently (Figure 1).
Dementia
Dementia is a syndrome characterized by disturbance of multiple brain functions, including memory, thinking, orientation, comprehension, calculation, learning capacity, language, and judgment. Consciousness is not clouded. The impairments of cognitive function are commonly accompanied, and occasionally preceded, by deterioration in emotional control, social behavior, or motivation [15]. Dementia can affect a person in different ways, and progression of the disease depends upon the impact of the disease itself and the person’s personality and state of health. Dementia can be divided in three stages.
• Early stage: First year or two.
• Middle stage: Second to fourth or fifth years.
• Late stage: Fifth year and after.
These periods are given as an approximate guideline and not all persons with dementia will display the same symptoms. Common symptoms experienced by people with dementia syndrome have been illustrated by Table 1.
| Early stage | Middle stage | Late stage |
|---|---|---|
| The early stage is often overlooked. Relatives and friends (and sometimes professionals as well) see it as "old age", just a normal part of ageing process. Because the onset of the disease is gradual, it is difficult to be sure exactly when it begins. | As the disease progresses, limitations become clearer and more restricting. | The last stage is one of nearly total dependence and inactivity. Memory disturbances are very serious and the physical side of the disease becomes more obvious. |
| Become forgetful, especially regarding things that just happened | Become very forgetful, especially of recent events and people's names. | Usually unaware of time and place. |
| May have some difficulty with communication, such as difficulty in finding words. | Have difficulty comprehending time, date, place and events; may become lost at home as well as in the community. | Have difficulty understanding what is happening around them. |
| Become lost in familiar places. | Have increasing difficulty with communication (speech and comprehension). | Unable to recognize relatives, friends and familiar objects. |
| Lose track of the time, including time of day, month, year, season. | Need help with personal care (i.e. toileting, washing, dressing) | Unable to eat without assistance, may have difficulty in swallowing. |
| Have difficulty making decisions and handling personal finances. | Unable to successfully prepare food, cook, clean or shop. | Increasing need for assisted self-care (bathing and toileting). |
| Mood and behaviour: May become less active and motivated and lose interest in activities and hobbies may show mood changes, including depression or anxiety may react unusually angrily or aggressively on occasion. | Unable to live alone safely without considerable support. | May have bladder and bowel incontinence. |
| Behaviour changes may include wandering, repeated questioning, calling out, clinging, disturbed sleeping, hallucinations (seeing or hearing things which are not there). | Change in mobility, may be unable to walk or be confined to a wheelchair or bed. | |
| May display inappropriate behaviour in the home or in the community (e.g. disinhibition, aggression). | Behavior changes, may escalate and include aggression towards career, nonverbal agitation (kicking). |
Table 1. Common symptoms experienced by people with dementia syndrome.
What causes Alzheimer’s disease?
So far, no one single factor has been identified as a cause for Alzheimer’s disease. It is likely that a combination of factors, including age, genetic inheritance, environmental factors, lifestyle and overall general health, are responsible. In some people, the disease may develop silently for many years before symptoms appear.
Age
Age is the greatest risk factor for dementia. Dementia affects one in 14 people over the age of 65 and one in six over the age of 80. However, dementia is not restricted to older people: in the UK, there are over 17,000 people under the age of 65 with dementia, although this figure is likely to be an underestimate.
Genetic inheritance
Many people fear that they may inherit Alzheimer’s disease and scientists are currently investigating the genetic background to Alzheimer’s. We do know that there are a few families where there is a very clear inheritance of the disease from one generation to the next. This is often in families where the disease appears relatively early in life. In the vast majority of cases, however, the influence of inherited genes for Alzheimer’s disease in older people seems to be small. If a parent or other relative has Alzheimer’s, your own chances of developing the disease are only a little higher than if there were no cases of Alzheimer’s in the immediate family [16].
Other factors
Because of the difference in their chromosomal make-up, people with Down ’s syndrome who live into their 50’s and 60’s are at particular risk of developing Alzheimer’s disease. People who have had severe head or whiplash injuries also appear to be at increased risk of developing dementia. Boxers who receive continual blows to the head are at risk too. Research has also shown that people who smoke, and those who have high blood pressure, high cholesterol levels or diabetes, are at increased risk of developing Alzheimer’s. You can help reduce your risk by not smoking, eating a healthy balanced diet and having regular checks for blood pressure and cholesterol from middle age. Maintaining a healthy weight and leading an active lifestyle combining physical, social and mental activity will also help.
Symptoms
People in the early stages of Alzheimer’s disease may experience lapses of memory and have problems finding the right words. As the disease progresses, they may: Become confused and frequently forget the names of people, places, appointments and recent events experience mood swings, feel sad or angry, or scared and frustrated by their increasing memory loss become more withdrawn, due either to a loss of confidence or to communication problems have difficulty carrying out everyday activities they may get muddled checking their change at the shops or become unsure how to work the TV remote (Figure 2).
Epidemiology of AD
AD is a critical public health issue in the United States and many other countries around the world, with a significant health, social, and financial burden on society. An estimated 5 million Americans have AD, with a new diagnosis being made every 68 sec. In the United States, AD is the fifth leading cause of death among older adults, and about $200 billion are spent annually on direct care of individuals living with dementia. Worldwide, it is estimated that 35 million people have AD or other types of dementia, and about 65 million people are expected to have dementia by 2030 (115 million by 2050). AD is a multi-factorial disease, with no single cause known, and several modifiable and non-modifiable risk factors are associated with its development and progression. Age is the greatest risk factor for the development of AD. The likelihood of developing AD increases exponentially with age, approximately doubling every 5 years after age 65. The vast majority of individuals suffering from AD are aged 65 or older and have ‘late-onset’ or ‘sporadic’ AD (95% of all cases). Rare genetic mutations are associated with the development of AD before age 65, which is known as ‘early onset ‘or ‘familial’ AD (B5% of all cases). People with familial forms of AD have an auto somal dominant mutation in either one of the presenil in genes located on chromosomes 1 and 14 or in the Amyloid Precursor Protein (APP) gene located on chromosome 21. In addition, individuals with Down’s syndrome (trisomy 21) have an increased risk of developing early onset AD. The genetics of sporadic AD are more complex and less well understood. It is known that the epsilon fourallele of the polipoprotein E (APOE) gene located on chromosome 19 is a risk factor for the development of sporadic AD. The prevalence of AD is higher among females, reflecting the longer life expectancy of women. Lower educational attainment has been associated with increased risk of AD dementia,10 consistent with the idea that education serves to increase a person’ s cognitive reserve and resilience to AD pathology. Alarge body of evidence suggests that cerebra vascular risk factors play a significant role in both the development and progression of AD; people with a history of diabetes, hypertension, obesity, and smoking have a substantially elevated risk of AD. Family history of AD in first-degree relatives and a history of head injury with loss of consciousness are also risk factors for the development of AD [17].
Pathology
The pathological hallmark of Alzheimer’s disease is the presence of amyloid plaques and Neurofibrillary Tangles (NFT). There is diffuse atrophy of the cerebral cortex and secondary dilatation of the ventricles. The deposits are found more at the hippocampus, temporal cortex and nucleus basalis of meyernet. There is loss of neurons due to the pathological changes leading on to reduced levels of neurotransmitters especially acetylcholine causing cognitive deficits in these patients. The widely accepted among them are,
• Amyloid cascade hypothesis.
• Tau hypothesis.
• Mitochondrial cascade hypothesis.
Amyloid cascade hypothesis: This is the most widely accepted hypothesis. The deposition of Aβ42-amyloid plaques in the brain is considered the basic pathology. Aβ42 is derived from Amyloid Precursor Protein (APP) by the sequential action of β-secretase and γ-secretase. Aβ42 is insoluble and aggregates to form plaques which causes oxidative damage and initiates inflammatory processes leading on to neuronal death. There is hyper phosphorylation of tau proteins and their deposition as neurofibrillary tangles secondary to amyloid deposition. Alzheimer’s disease occurs in two forms: Familial and sporadic forms. Familial forms have an early onset and are associated with mutations in APP gene (chromosome 21), presenillin-1 (chromosome 14) and presenillin-2 genes (chromosome 1). The late onset familial form and sporadic forms of AD are associated with the presence of ApoE4 allele. ApoE is involved in cholesterol transport and has three alleles 2, 3 and 4. ApoE4 allele is present in 40-80% of the Alzheimer’s patients, though the normal distribution in Caucasian population is only 24-30%. ApoE4 is shown to increase the production and decrease the clearance of amyloid.
Tau hypothesis: The amyloid cascade hypothesis does not satisfactorily explain sporadic cases of Alzheimer’s disease and the level of amyloid deposits does not correlate with the degree of cognitive decline. This lead to the Tau hypothesis which asserts that the deposition of tau and formation of neurofibrillary tangles is the basic pathology and the amyloid deposition occur secondary to it. Tau is a microtubule associated protein which binds to and stabilizes the microtubules involved in intracellular transport. The hyper phosphorylation of tau reduces the binding of tau to microtubules and the sequestration of hyper phosphorylated tau into Neurofibrillary Tangles (NFTs) reduces the amount of tau that is available to bind microtubules. As a result the microtubules disintegrate leading to reduced axonal transport and cell death [18].
Mitochondrial cascade hypothesis: The reduced mitochondrial function to handle the free radicals is considered the initiating step in Alzheimer’s disease.
Diagnosis of AD
In clinical settings, the diagnosis of AD is largely based on medical history, physical and neurological examinations, and neuropsychological evaluation, as well as the exclusion of other etiologies using selective ancillary testing. The clinical diagnosis of AD has an accuracy of 70%-90% relative to the pathological diagnosis, with greater accuracies being achieved in specialty settings such as memory disorder clinics.
The cornerstone of the clinical diagnosis is a set of consensus criteria first established in 1984 and last updated in 2011 by the National Institute on Aging Alzheimer’s Association (NIAAA) workgroup. When the patient’s cognitive impairment has an atypical clinical course or is suspected to be due to other etiologiesin addition to AD, the diagnosis of ‘possible’ AD dementia is recommended. Patients with AD generally have normal findings on physical and neurological examinations. To help with the differential diagnosis, Table 2 summarizes some of the clinical features that distinguish AD [19].
Establishing the diagnosis of Alzheimer disease
Establishing the diagnosis of Alzheimer disease relies on clinical neuro pathologic assessment. Neuropathology findings on autopsy examination remain the gold standard for diagnosis of AD. The clinical diagnosis of AD (prior to autopsy confirmation) is correct approximately 80%-90% of the time.
• Clinical signs: Slowly progressive dementia.
• Neuroimaging.
• Gross cerebral cortical atrophy on CT or MRI.
• Diffuse cerebral hypo metabolism on PET.
• Neuro pathologic findings: Microscopic β-amyloid neuritic plaques, intraneuronal neurofibrillary tangles (containing tau protein), and amyloid angiopathy at postmortem examination. The plaques should stain positively with β-amyloid antibodies and negative for prion antibodies, which are diagnostic of prion diseases. The numbers of plaques and tangles must exceed those found in age-matched controls without dementia. Guidelines for the quantitative assessment of these changes exist.
• Cerebrospinal Fluid (CSF): Decrease Aβ amyloid 42 and increased tau.
| Sr. no. | Clinical feature | Alzheimer’s dementia | Vascular dementia | Parkinson’s dementia | Dementia with Lewy bodies | Frontotemporal dementia |
|---|---|---|---|---|---|---|
| 1 | Patient profile | >65 years old | >40 years old vascular risk factors | >65 years old | 75 years old (mean) | 50-70 years old 50% autosomal dominant |
| 2 | History | Gradual onset and deterioration | Acute onset, stepwise deterioration | Gradual onset and deterioration | Gradual onset and deterioration | Gradual onset and deterioration |
| 3 | Initial symptoms | Memory loss | Executive dysfunction | Visual hallucinations | Visual hallucinations fluctuating attention | Memory intact disinhibition, apathy or aphasia |
| 4 | Physical findings | No motor impairment (until late stage) | Pyramidal (upper motor neuron) signs | Parkinsonism (preedes dementia by>1 year) | Parkinsonism (presents within 1 year of dementia) | Usually none (rarely associated with motor neuron disease) |
Table 2. Clinical features that distinguish AD from other dementias.
Neuropathology and clinical signs of Alzheimer’s disease
The clinical diagnosis of Alzheimer’s disease is said to be correct 75% to 90% of the time. According to, accuracy is highest for neurologists specializing in memory disorders and lowest for general practitioners, who have a tendency to over diagnose Alzheimer’s disease. The clinical accuracy also tends to be lower for older patients’ who often have mixed pathology rather than a single cause of dementia. The only clinical means of establishing a definite diagnosis is by microscopic examination of brain tissue as there are no laboratory tests and neither sophisticated imaging techniques nor detailed neuropsychological evaluation can specify Alzheimer’s disease categorically. Typically, the onset is from 40 years of age onwards with insidious degeneration until death at about sixty years following onset. The brain invariably displays a degree of atrophy; however, age associated atrophy and the normal variability in brain size preclude a diagnosis based solely on gross examination of the brain. Atrophy of the medial portion of the temporal lobe is often disproportionate to other areas of the cortex. In most cases, the primary sensory and motor cortices are relatively spared and on sectioning the brain, the lateral ventricles are usually dilated and the hippocampus and amygdale are atrophic. More specific neuronal alterations accompany neuronal and synaptic loss. The most important of these alterations is paired helical filaments which are intra neuronal proteinaceous structures that are composed by an abnormal form of tau protein. The neuropathological hallmarks of Alzheimer’s disease are the intracellular neurofibrillary tangles of tau protein and amyloid plaques, primarily composed of aggregated amyloid beta peptide [20]. At high concentrations vesicular amyloid beta aggregates to form high molecular weight species which are capable of seeding amyloid fibril growth suggest that it is the segregate that seeds the extracellular amyloid plaque formation seen in the pathogenesis of Alzheimer’s disease (Table 3).
| Antecedent | Direction | Possible mechanism |
|---|---|---|
| Cardiovascular disease | Increased | Parenchymal destruction strategic location “↑”beta (symbol) deposition |
| Smoking | Increased | Cerebrovascular effects oxidative stress |
| Hypertension | Increased and decreased | Cerebrovascular disease |
| Type II diabetes | Increased | Insulin and A beta (symbol) compete for clearance |
| Obesity | Increased | Increased risk of type II diabetes inflammatory |
| Traumatic head injury | Increased | “↑”a beta (symbol) and amyloid precursor protein deposition |
| Education | Decreased | Provides cognitive reserve |
| Leisure activity | Decreased | Improves lipid metabolism, mental stimulation |
| Mediterranean diet | Decreased | Antioxidant, anti-inflammatory |
| Physical activity | Decreased | Activates brain plasticity, promotes brain vascularization |
| Source: Epidomology of Alzeimers disease | ||
Table 3. Factor that modify the risk of Alzheimer disease.
Impact on health care
The annual healthcare costs of AD in the United States have been estimated to be as high $100 billion. In Japan, the annual healthcare cost of AD is probably much smaller compared to the US. However, with the increasing elderly population in Japan, the number of elderly individuals with AD may also be increasing in frequency. It is therefore inevitable that sooner or later, Japanese health authorities will have to confront increasing healthcare figures related to AD. In addition to the impact on healthcare budget, there is also the emotional as well as physical stress brought to the family of the AD patient. While relatives and caregivers of elderly AD patients have the will to care for them, family care seems to break down sooner or later. Traditionally, the Japanese have had a unique attitude toward misfortune and burden. As a result, many caregivers in Japan endured the care burden because most have accepted it as their fate. But this traditional attitude is slowly fading as more and younger caregivers in modern Japanese society are choosing not to undertake home care but opt for institutionalization.
Pathogenic aspect
Because the origin of AD is still unknown, a universal concept on the pathophysiology of the disease remains a debatable issue. However, two pathological hallmarks of the disease have been identified, i.e., neuritic plaques and Neurofibrillary Tangles (NFTs). Amyloid protein is a major component of the neuritic plaques. These plaques accumulate extracellularly in the brain. The neuritic senile plaque consists of a fibrillar amyloid core surrounded by dystrophic neurites and reactive microglia. NFTs develop within the soma of the neuron and after degeneration of the parent cell convert into extraneuronal structures, and are finally engulfed and degraded by astrocytes. The NFTs are composed of paired helical filaments microtubule. There is a major debate on whether amyloid plaques are the cause of neurodegeneration or simply an end stage of amyloid fibril build-up at the cellular level, there is a marked reduction in the levels of neurotransmitters, e.g., acetylcholine, serotonin, noradrenaline, dopamine, glutamate and substance P. In this dramatic and global reduction of neurotransmitters, the depletion of acetylcholine is the most important event.
Causes of Alzheimer’s disease
At present AD is considered a multi factorial disease with a combination of aging, genetic and/or environmental factors triggering the pathological decline. However, the precise mechanisms causing the disease are still unknown. Clinically, increasing age and a positive family history of dementia are the only definite risk factors for AD. And recent studies have shown that the presence of Apoliprotein E (ApoE) type 4 allele is also a potential risk factor.
Development and treatment of synthetic drugs
Numerous drugs have been studied as potential treatments for AD. But with the actual cause of the disease yet to be identified, drug development in this area has been confined to limiting the progression of the disease. At the moment, drug development has focused on (i) Symptomatic treatments aimed at relenting deficient neurotransmitters, and (ii) Etiologically based treatments aimed at slowing or halting the rate of progression.
Cholinergic system and Alzheimer’s disease
The most consistent neurotransmitter related change in the brain of an AD patient is the dramatic decrease in cholinergic innervation in the cortex and hippocampus due to the loss of neurons in the basal forebrain. This fact has been confirmed in a large number of animal and human studies. This loss of cholinergic neurons and the associated decrease in levels of cholinergic neurotransmission have been associated with the cognitive impairment seen in AD patients.
AChE inhibitors
Different types of AChE inhibitors have been studied for the treatment of AD. Some of the AChE inhibitors described below differ in their mechanism of action, metabolism and brain selectivity. Donepezil hydrochloride (E2020) is discussed in detail in section 5.
Physostigmine
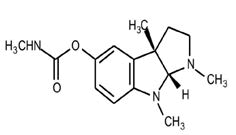
Chemical formula: C15H21N3O2
IUPAC: [(3aR, 8bS)-3,4, 8b-trimethyl-2,3a-dihydro-1H-pyrrolo[2,3-b]indol-7-yl] N-methyl carbamate
MOA: Physostigmine (PHY), a cholinesterase inhibitor developed by Pfizer, is one of the first drugs to show cognitive improvements for some AD patients in 11 studies conducted. The results of an early review of these studies showed certain degree of improvements in 5 investigations using parenteral administration and in 4 of the 5 using oral administration. However, further studies show that this is a short acting AChE inhibitor.
November 1998, the US FDA issued a non-approval letter for PHY's Alzheimer's indication based mainly on a lack of efficacy as shown from results in phase II and phase III studies.
Tacrine
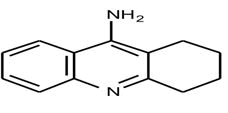
Chemical formula: C13H14N2
IUPAC: 1,2,3,4-tetrahydroacridin-9-amine;hydrochloride
Tacrine (THA/Cognex) is the first drug approved by the U.S. FDA for the palliative treatment of mild to moderate AD. Tacrine is an amino acridine compound which is centrally active and a reversible.
MOA: AChE inhibitor with a moderately long duration of action. Monitored for ALT levels in order to prevent the possibility of hepatotoxicity. In an early study conducted by Summers, et al. In 1986, the patients receiving tacrine showed a small, but nonetheless significant reduction in the decline of cognitive performance (2.4 points in ADAS-cog) compared to placebo. These results led to a larger multicenter study carried out during the period 1990-1994 involving a total of 1905 patients enrolled in six major double blind, placebo controlled trials using similar methods of assessment of cognitive function. On the basis of comparisons with placebo in cognitive scoring, mental deterioration was arrested by 2 to 12 months according to Mini Mental State Examination (MMSE) and 5 to 6 months according to the Alzheimer's Disease Assessment Scale (ADAS) when tacrine treatments continued for 2 to 6 months. A dose response effect (20 to 80 mg per day) was described with a 4 points improvement on the ADAS cognitive scale after 3 months' treatment. In a 30 week, randomized, controlled trial carried out with increasing doses of tacrine (up to 160 mg/day) the resulting observation was a significant, dose related improvement in objective performance based tests, clinician and caregiver rated global evaluation and measures of quality of life. However, a high proportion of patients showed increased levels of serum alanine amino transferase which is indicative of hepatocellular injury. In summary; tacrine can modestly improve cognitive function in a portion of patients who are able to tolerate it. Given the propensity of this drug to cause marked increases on alanine aminotransferase levels, patients receiving this compound must be carefully monitored for ALT levels in order to prevent the possibility of hepatotoxicity. Because of the positive effects observed in tacrine, this compound has been used as the reference drug in the clinical development of other AChE inhibitors for both clinical efficacy and side effects. Several tacrine analogs are under preclinical or clinical evaluation and some of these are presented below.
Velnacrine
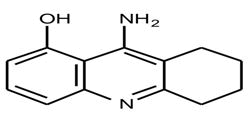
Chemical formula: C13H14N2O
IUPAC: 9-amino-1,2,3,4-tetrahydroacridin-1-ol
MOA: Velnacrine (HP-029) is a hydroxy metabolite of tacrine, with a shorter half-life. This compound acts biochemically as a potent AChE inhibitor. Pharmacodynamic trials with single doses of this compound in both healthy young individuals and patients with AD demonstrated statistically significant cognitive improvements compare. However, as much as 20-30% of patients exposed to this drug developed hepatotoxicity.
Amiridine
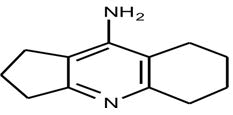
Chemical formula: C2H5N
IUPAC: Amiridine
MOA: Amiridine (NIK-247, Senita), another tacrine derivative AChE inhibitor, is now under phase III study in Japan. Animal studies of this compound show increase acetylcholine levels as measured during in vitro and in vivo experiment. In a passive avoidance test on rats with experimentally induced amnesia, amiridine improved cognitive function at different levels of learning and memory processes. The compound was administered orally before or after training at doses ranging from 0.1 to 3 mg/kg. The results of this study show that amiridine may have more than one memory enhancing mechanism, one at low doses and the other at high doses. A clinical study of this compound was conducted in a group of 88 patients with AD. Amiridine was administered to 74 patients (at doses of 20, 40, or 60 mg/day) and the remaining 14 patients make up the control group. The treatment period lasted for 14 months, with a follow-up period that included clinical observation and testing. Results of this study show that amiridine had well defined therapeutic effects in 30-40% of patients treated. Cognitive functions and general mental status of the patients continued to improve or were stabilized in 14 months while speech improved for a shorter period of time. Beneficial effects were produced at both the initial and marked stages of the disease, although the most significant results were obtained in patients with unmarked dementia.
Eptastigmine
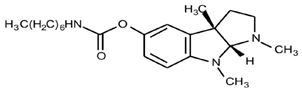
Chemical formula: C21H33N3O2
IUPAC: [(3aR,8bS)-3,4,8b-trimethyl-2,3a-dihydro-1H-pyrrolo[2,3-b]indol-7-yl] N heptyl carbamate
MOA: Eptastigmine (heptylphysostigmine, MF 201, L693487) is an alkaloid derivative of physostigmine. Compared to physostigmine and tacrine, eptastigmine has a much longer duration of action. In a study conducted by Troetel, et al. It is found that the drug inhibits red blood cell AChE in a dose dependent fashion. The mean AChE recovery half-life was about 10 h, with a mean residual inhibition of 13% 24 h after a 30 mg dose. Phase II studies in Alzheimer's patients indicate that doses of 40-60 mg per day of eptastigmine are relatively safe and well tolerated and that moderate AChE inhibition (30-40%) are associated with maximal cognitive efficacy. In the first phase III study carried out using doses up to 15 mg. t.i.d. for 25 weeks, the drug is still shown to be well tolerated in AD patients and appears to affect their cognitive and functional performance. The positive effects of eptastigmine compared to placebo appear to be greater in the more severely impaired patients.
Galanthamine
Chemical formula: C17H21NO3
IUPAC: 5,6,9,10,11,12- hexahydro- 3-methoxy- 11-methyl- 4aH- [1]benzofuro[3a,3,2-ef] [2] benzazepin- 6-ol
MOA: Galanthamineis a tertiary alkaloid originating from botanical sources. As early as the 1950’s, this compound was used by Bulgarian and Russian scientists in post-surgery reversal of tubocurarine induced muscle relaxation, muscular dystrophy and traumatic brain injury. In 1972, soviet researchers had demonstrated that galanthamine could reverse scopolamine induced amnesia in mice. This finding was later on extended to humans. Despite the substantial and long lasting history of clinical use of this compound in humans, it was not until 1986 when this compound was studied for the treatment of AD. The limited use of this compound in clinical studies may be attributed to the fact that all supplies came from natural extracts and were only available in very limited amounts. It was not until 1960 when the chemical synthesis of this compound was accomplished leading to the industrial scale production and thus allowing drug development without the limitations imposed by the natural sources.
Animal studies identify galanthamine as a reversible AChE inhibitor with differential activity on the central nervous system and hence an ability to cross the blood brain barrier. In human studies, the drug has shown promise in the treatment of patients with Senile Dementia of Alzheimer Type (SDAT). The interim results obtained from Phase II study confirm earlier reports that galanthamine holds promise as an effective and welltolerated treatment for cognitive impairment in patients with SDAT galanthamine is approved in Austria for AD indication. It is currently in phase III studies in Europe, USA, Australia, Canada and other countries.
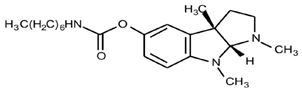
Rivastigmine
Chemical formula: C14H22N2O2
IUPAC: [3-((1S)-1-(dimethylamino) ethyl] phenyl) N-ethyl-N-methylcarbamate
MOA: Rivastigmine (SDZ-ENA-713/Exelon) is a miotine derivative of physostigmine. This compound is a carbamate type AChE inhibitor with a short kinetic half-life and duration of action of approximately 10 h. This carbamate inhibit AChE by carbamoylating the serine residue of the catalytic triad in a pseudoirreversible manner.
In phase III clinical studies conducted in the US, it was reported that patients receiving the highest doses of this compound (6-12 mg/day) showed average improvement of 0.79 points in the ADAS-cog scale, compared with an average decline of 4.15 points in the placebo group. The low dose group showed a decline of 2.2 points, intermediate between placebo and high dose groups. In the CIBIC-plus scale, improvement was observed in 24% of the patients receiving the high dose, 25% on the low dose and 16% in the placebo group. About 25% of drug treated patients showed side effects such as nausea, vomiting, diarrhea, loss of appetite, dizziness and fatigue. Based on these findings, a regimen of increasing dosage seems to be necessary in order to achieve maximum clinical benefits with minimal side effects.
Rivastigmine is approved in more than thirty countries worldwide under the trade name Exelon. It has been launched in Europe, Latin America, Asia, Africa and some Middle East countries. In July 1998, the US FDA requested additional analyses of data to confirm safety but no additional trials were requested. The launching of this product in the US is expected by the middle of this year 1999.
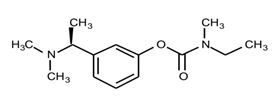
Metrifonate
Chemical formula: C4H8Cl3O4P
IUPAC: (2,2,2-Trichloro-1-hydroxyethyl) phosphonate de dimethyle
Metrifonate is an organophosphorous compound originally used as an antihelmintic drug. It is not aAChE inhibitor in itself but is time-dependently transformed into a physiologically active AChE inhibitor by dehydrochlorination. This compound is converted nonenzymatically to the active metabolite 2,2-dimethyl Dichlorovinylphosphate (DDVP). DDVP is shown to increase ACh levels by stably binding to the active site of the AChE enzyme, leading to a sustained enzyme inhibition over time. Metrifonate has a short plasma half-life but has a long duration of action in the brain. These characteristics make it a unique compound among the AChE inhibitors being used or studied for the treatment of AD. Studies performed on laboratory animals show that metrifonate improve the cognitive performance of animals in various behavioral models. This compound is observed to readily enter the animal brains and dose dependently inhibit AChE activity. As a consequence of AChE inhibition, metrifonate increases extracellular acetylcholine levels in the brain, local cerebral glucose utilization, and the cortical EEG activity in rat models.
The first application of metrifonate in AD therapy was studied by Beckel, et al. In this study, it was reported that metrifonate significantly improved cognitive function on the ADAS-cog scale and inhibited the erythrocyte AChE activity to 55.9% of control levels. In a 3-month dose finding study. Metrifonate improved the cognitive and global function of probably AD patients. In this study, a once daily metrifonate dose of 30-60 mg, based on weight, improved ADAS-cog and CIBIC-plus scores in the intent to treat patient population by 2.94 and 0.34 points, respectively, at 12 weeks of treatment in comparison with placebo. Adverse reactions observed during this study were generally transient and mild in intensity. A prospective 6 months study conducted by Morris, et al. confirms the finding of the earlier study and extends it by demonstrating that the efficacy of metrifonate was sustained over the longer treatment period.
(-)-Huperzine A
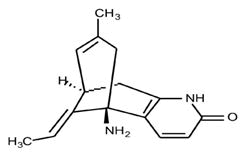
Chemical formula: C15H18N2O
IUPAC: 1-amino-13-ethylidene-11-methyl-6-azatricyclo[7.3.1.02,7]trideca-2(7),3,10-trien-5-one
MOA: (-)-Huperzine A (HupA) is another kind of AChE inhibitor derived from natural extracts. It is an alkaloid isolated from the club moss, Huperzia serrata, which has gained popularity in Chinese herbal medicine. The compound's unique pharmacological features and relative lack of toxicity makes it a potent compound for AD treatment. The structure of racemic Huperzine A shows some similarity to other known AChE inhibitors. Animal studies reveal significant cognitive enhancement. Initial clinical trials have established the safeness of HupA and provided preliminary evidence for significant effects on patients exhibiting dementia and memory disorders. In a recent study conducted by Koenig, et al. It was demonstrated that HupA decreases neuronal cell death caused by glutamate, particularly in primary cultures derived from hippocampus and cerebellum of embryonic rat. Because this compound is shown to increase acetylcholine levels in the brain and at the same time decrease neuronal death, HupA may be an important and promising drug for the treatment of AD.
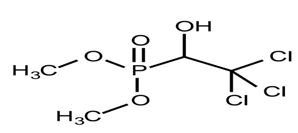
Donepezil hydrochloride
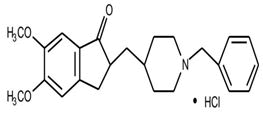
Chemical formula: C24H30ClNO3
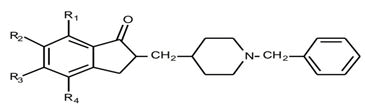
IUPAC: 2-[(1-benzylpiperidin-4-yl) methyl]-5,6-dimethoxy-2,3-dihydroinden-1-one; hydrochloride
Discovery of donepezil hydrochloride
Donepezil hydrochloride (E2020) is the second drug approved by the US. FDA for the treatment of mild to moderate AD. It is a new class of AChE inhibitor having an N-benzylpiperidine and an indanone moiety which shows longer and more selective action. It is now marketed in the U.S. and in some European and Asian countries under the trade name of Aricept. In Japan, Aricept is now under application to the ministry of Welfare.
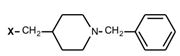
The research on E2020 started in 1983. Following research developments of tacrine, our group in Eisai started to develop tacrine derivatives. However, we failed to develop a non-toxic tacrine derivative. Through random screening, we encountered N-benzylpiperazine derivative 1 which was then originally being synthesized in the study of anti-arterial sclerosis. Our tests showed that the acetylcholinesterase activity of N-benzylpiperazine derivative was 12.6 mM at IC50 in rat brain homogenate. This was not very strong but the compound's novel structure was very promising. We decided to use N-benzylpiperazine derivative as the seed compound and synthesized about 700 derivatives. Our succeeding experiments showed a dramatic increase in anti-acetylcholinesterase activity when N-benzylpiperazine was replaced with N-benzylpiperidine (Figure 3). It was a quantum leap in our investigation.
Next challenge was to replace the ether moiety with an amide moiety. This process also increased antiacetyl cholinesterase activity. We thought that the introduction of a functional group at the para-position of the benzamide group might increase potency but removal of the nitro group at the para-position decreased the potency of the compound.
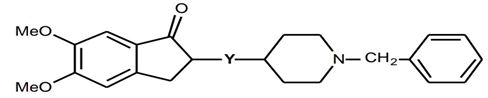
On the basis of these findings, we synthesized benzamide derivatives. We later on discovered that benzylsulfonyl derivative 4 was the most potent AChE inhibitor with an anti-AChE activity 21,000 fold greater compared to the seed compound 1. However, our excitement was shortlived because we found that this compound has a very poor bioavailability rate and has a short duration of action and therefore could not be a candidate for clinical testing but this benzylsulfonyl derivative has a novel chemical structure and has a selective affinity to AChE, making it a very attractive lead compound. Immediately after these findings, we started the screening process again our next strategy in drug design was the replacement of the amide moiety with ketone moiety 7. This approach maintained the AChE activity of the compound. Furthermore, this cyclic-amide derivative 6 showed enhanced inhibitory action. On the basis of these results, an indanone derivative 8 was designed. The resulting AChE activity was moderate, but we achieved longer duration of action. Subsequently, various indanone derivatives were synthesized and tested for anti-AChE activity. Among the indanone derivatives that were developed, donepezil was found to be the best balanced compound (Figure 4).
Structure-Activity Relationships (SAR)
The indanone derivatives were tested for in vitro inhibition of AChE. A rat brain homogenate was used as the AChE source and the activities were measured according to the method of Ellman, et al. The indanone derivative was divided into four parts as shown in Figure 5 part 1 (indanone moiety), part 2 (linkage moiety), part 3 (piperidine moiety), and part 4 (benzyl moiety). All data were obtained from the racemic compounds.
Table 4 shows the anti-AChE activity of derivatives from the indanone moiety with various bicyclic rings. The effect of replacement of indanone ring with a-tetralone, 1-benzosuberone, 5,6-dimethoxy-1-indanone, 5,6-indanol, 5,6-dimetoxyindene was measured. The ring expansion of cyclic ketone (i.e. compounds 1 0, 1 1) greatly decreased the activity. But the introduction of the methoxy group to the 5,6-position of the indanone moiety increased the activity by 25-fold (E2020). The carbonyl group of the indanone moiety is essential to the activity since the indanol (12) and indene (13) derivatives both showed decreased potency.
 |
||
|---|---|---|
| Compound no. | Inhibition of AChE IC50(nM)a | |
| 9 | 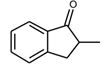 |
150 |
| 10 | 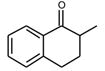 |
2100 |
| 11 | 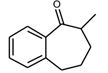 |
15000 |
| E2020 | 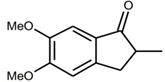 |
5.7 |
| 12 | 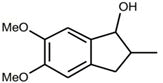 |
300 |
| 13 | 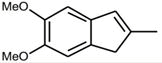 |
4400 |
| Note: a: Deviation of measurement of IC50 value is 10-20%. | ||
Table 4. Anti-AChE Activity of part 1 substituted compound (1).
The effect of introducing one or more methoxy groups in the indanone moiety is shown Table 5. We observed that the introduction of a methoxy group at the R3-position increased the activity by 20-fold (15). A methoxy substituent at the R4-position increased the activity by 10-fold (16) while substitution at the R2.
 |
|||||
|---|---|---|---|---|---|
| Compound no. | R1 | R2 | R3 | R4 | Inhibition of AChE IC50(nM)a |
| 9 | H | H | H | H | 150 |
| 14 | H | OMe | H | H | 81 |
| 15 | H | H | OMe | H | 6.4 |
| 16 | H | H | H | OMe | 12 |
| E2020 | H | OMe | OMe | H | 5 |
| 17 | OMe | OMe | H | H | 85 |
| 18 | OMe | H | OMe | H | 25 |
| 19 | OMe | H | H | OMe | 36 |
| 20 | H | H | OMe | OMe | 20 |
| 21 | OMe | OMe | OMe | H | 13 |
| Note: a: Deviation of mesurement of IC50 value is 10%-20% | |||||
Table 5. Anti-AChE Activity of part 1 substituted compound (2).
Position (14) results in slightly increased activity. These results suggested that the methoxy group at the paraposition in the carbonyl group of the benzoyl moiety greatly enhanced binding to the active site of the AChE enzyme. Among these derivatives, 5,6-dimethoxylindanone derivative or the E2020, showed the highest activity.
Various bridging groups between the indanone moiety and the piperidine moiety were tested. The results are shown in Table 6. Direct connection of the indanone and the piperadine rings dramatically decreased potency (22). The effect of the length of the bridging moiety on potency varied in the following order: propylene (26)>methylene (E2020)>pentylene (28)> ethylene (25)>butylene (27). The introduction of an exo-methylene double bond on both the indanone and piperidine moiety decreased the activity (23,24).
 |
||
|---|---|---|
| Compound no. | Y | Inhibition of AChE IC50(nM)a |
| E2020 | CH2 | 5.7 |
| 22 | - | 3300 |
| 23 | =CH2 | 13 |
| 24 | CH2= | 90 |
| 25 | CH2CH2 | 30 |
| 26 | CH2CH2CH2 | 1.5 |
| 27 | CH2CH2CH2CH2 | 35 |
| 28 | CH2CH2CH2CH2CH2 | 14 |
| Note: a: Deviation of measurement of IC50 value is 10-20% | ||
Table 6. Anti-AChE activity of part 2 substituted compound
Table 7 shows the relationships between the location and the number of nitrogen atom and activity. The nitrogen atom at 1-position of the benzylpiperidine moiety was very important since the activity of 4-benzylpiperidine derivative (29) largely decreased activity. Replacement of the piperidine group with a piperazine group (30) also resulted in decreased potency. The distance between the carbonyl group in indanone ring and the nitrogen atom in piperidine ring might be critical for anti-AChE activity.
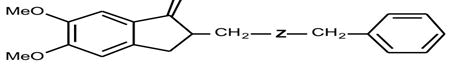 |
||
|---|---|---|
| Compound no. | Z | Inhibition of AChE IC50 (nM)a |
| E2020 | 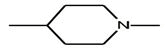 |
5.7 |
| 29 | 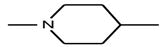 |
480 |
| 30 | 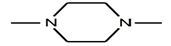 |
94 |
| Note: a. Deviation of measurement of IC50 value is 10%-20% | ||
Table 7. Anti-AChE activity of part 3 substituted compound.
Table 7 shows the relationships between the benzyl moieties. The 3-position-substituted benzyl derivatives showed the highest potency among the 2, 3, and 4-substituted regioisomers. Substitution of the benzene ring with an electron-donating methyl group and an electron withdrawing nitro group showed a similar effect. The basicity of the nitrogen atom in the piperidine ring appear to have an important effect in increasing activity since the N-benzoyl piperadine derivative (34) was almost inactive. Removal of the benzyl group (38) caused a great reduction in the potency of the compound but the activity was retained after replacement with cyclohexyl methyl group (39). The replacement of benzyl moiety with phenethyl (40) and 2-naphthyl group (41) decreased potency. Among the indanone derivatives, compound E2020 is one of the most potent compounds in terms of anti-AChE activity.
Donepezil as a selective AChE inhibitor
Donepezil was initially thought to be a mimic of ACh by structural similarity, and, therefore, a competitive inhibitor of AChE. The N-benzylpiperidines show outstanding in vitro selectivity for AChE. The IC50 of donepezil for AChE is 5.7 nM while the IC50 for BuChE (butyryl cholinesterase), is about 7000 nM, a selectivity ratio in excess of three orders of magnitude. Tacrine and physostigmine show poor selectivity having the same order of magnitude IC50s for both AChE and BuChE. Inhibition of BuChE, which is abundant in plasma, may be associated with potentiating peripheral side effects. Therefore, an AChE inhibitor which is essentially devoid of BuChE activity may display higher therapeutic indices than those which are also active BuChE inhibitors.
Other approaches in Alzheimer’s disease treatment
While AChE inhibitors can alleviate the symptoms of AD, one should give some thought on the limitations of these therapeutic agents. What is more important is to be able to develop a therapeutic agent that can actually cure the disease. However, the development of curative compounds is markedly limited by the fact that the etiology and pathogenesis of AD is still unclear. Yet the research should continue.
Briefly discussed below are other approaches currently being pursued in the treatment of AD, such as anti-inflammatory agents, anti-oxidants, estrogen replacement therapy, galanin receptor antagonist, and the anti-amyloid strategy?
Anti-inflammatory agents
The use of anti-inflammatory agents in the treatment of AD was pursued based on the large body of pathological evidence suggesting the presence of inflammations in AD brain. These inflammations can generate a self-propagating process in which different molecules (complement, cytokines, acute phase proteins) act, potentiating b-amyloid toxicity. A significant observation derived from a study conducted on the use of Non-Steroidal Anti- Inflammatory Drugs (NSAIDs) in treating elderly arthritic patients, is the low incidence of AD among these patients suggesting NSAIDs may delay neuronal degradation and limit the progression of the associated inflammation in AD.
Anti-oxidants
Several Central Nervous System (CNS) disorders including AD are thought to be related to changes in oxidative metabolism. Normally, the interaction of these compounds with molecules crucial for cellular viability is inhibited by endogenous anti-oxidant enzymes and free radical scavengers. However, when anti-oxidant defenses are inadequate, free radicals will produce cytotoxic damage to the cell membrane, enzymes and DNA by altering the electron number, the structure and the function of lipids, proteins, nucleic acids and other cellular constituents. Studies show that oxygen radicals initiate amyloid build-up leading to neurodegeneration. On the basis of this observation, anti-oxidants as a therapeutic approach to Alzheimer's disease have been pursued.
Vitamin compounds with anti-oxidant properties such as retinol (Vitamin A), ascorbic acid (Vitamin C) and tocopherol (Vitamin E) are now being studied as a potential therapeutic approach to AD.
Estrogen replacement therapy
Animal studies have provided evidence that estrogen stimulates nerve growth production. In over iectomized rats, ERT has been shown to:
• Restore and even enhance learning abilities.
• Prevent the decrease of neuronal choline uptake and choline acetyltransferase.
• Reduce the decline in nerve growth factor and brain-derived neurotrophic factor mRNA in those brain areas.
• Exert neuroprotective effects in a tissue culture model.
These observations led to the application of Estrogen Replacement Therapy (ERT) to prevent neuronal degeneration and cognitive decline. Studies conducted by Honjo, et al. and Hagion, et al. All confirmed the evidence that estrogen responsive subjects exhibited osteoporosis and lower serum estrogen levels prior to beginning estrogen replacement, which suggests that AD in some women. May be associated with systemic estrogen deficiency. Long-term prospective trials of estrogen in normal premenopausal women and in women with AD are now needed to substantiate these hypotheses.
Galanin receptor antagonist
Galanin is a 29-amino acid peptide abundant in the brain and peripheral tissues. This peptide and its receptors have been implicated in a variety of physiological processes such as food intake, pain, anxiety and depression, memory and neuroendocrine functions. Tatemotoet al. was the first to isolate this polypeptide from porcine intestine. Galanin appears to co-exist with several other neurotransmitters including ACh in the ventral forebrain. The interaction between galanin and acetylcholine has been a major focus in galanin research. Axonal plexuses innervating the ventral hippocampus and nucleus basalis have been described in rat, monkey and human and galanin inhibits the release of acetylcholine in these regions. In AD brain tissue, galanin hyperinnervation of cholinergic neurons in the nucleus basalis has been observed suggesting that cholinergic dysfunction in AD patients may be depressed further by plasticity in the galanin system. It is therefore attractive to speculate that galanin has a crucial role in the regulation of cholinergic function in forebrain pathways relevant to memory and may be involved in the cognitive dysfunctions associated with Alzheimer's disease.
Anti-amyloid strategy
As discussed in section-AChE mechanism of action, b-amyloid deposits are found to co-localize with cellular proteins leading to the assembly of Ab peptides and its aggregation into amyloid plaques. Because of its close relationship with the plaques and neurofibrillary tangles, b-amyloid has long been considered to be responsible for the development and the progression of the neurodegeneration in AD. But the processes that transform b-amyloid into potentially neurotoxic amyloid and its accumulation as senile plaques are still unclear. However, the discovery of its presence in AD brains provides insight as to possible therapeutic targets for AD. Research has focused on interventions to prevent the destruction of neurons and the disruption of brain function by b-amyloid. These include the administration of antioxidants and free radical scavengers to reduce further neural damage from deposits of b-amyloid, the activation of various growth factors to repair damaged cells and restore their functions, and the stimulation of the normal processing of the precursor protein not only to aid in neural repair but more importantly to prevent the formation of additional b-amyloid.
Ayurvedic preparation used in Alzheimer’s
Combining healthier lifestyle behaviours was associated with a substantially lower risk for Alzheimer’s disease in a study that included data from nearly 3,000 research participants. Those who adhered to four or all of the five specified healthy behaviours were found to have a 60% lower risk of Alzheimer’s. The behaviour was:
• Physical activity.
• No smoking.
• Light to moderate alcohol consumption.
• A high quality diet.
• Cognitive activities.
In the ayurvedic system of medicine, rasayana and panchkarma therapy are very useful in the management of dementia. The rasayana therapy has the property to check the presenile and senile dhatu vaigunya and kshaya (degeneration).
Drugs used as:
• Ashwagandha
• Turmeric
• Brahmi
• Shankhpushpi
• Gotu kola
• Guggul
• Maidenhair tree
• Ginseng root
• Sage
• Galantamine
• Bhringaraj
• Vinpocetine
• Saffron
Ashwagandha (Withania somnifera)
Family: Solanaceae
Withania somnifera has been described as a nervine Tonic.
In Ayurveda and that is why it is a frequent ingredient of ayurvedic tonics, rejuvenators and vitalizer appear to ally disorders and prompt immunity and longevity in the users. The assessment of cholinesterase inhibition Was carried out by the usage of a colorimetric method based totally on Ellman’s response and demonstrated that the W. Somnifera extract substantially inhibited AChE in an awareness-dependent manner. Withania somnifera has been proven to slow, give up reverse and take away neuritic atrophy and synaptic loss, which is the main motive for neurodegenerative issues including alzheimer’s and dementia as confirmed by several clinical studies. Therefore, this herb can be used for the treatment and management of patients with AD. It improves the growth of new dendrites of neurons. Glycowithanolides withaferin-A and sitoindosides VII-X isolated from the roots of Withania somnifera have been shown to significantly reverse the ibotenic acid-induced cognitive defects in the AD model (Figure 6).
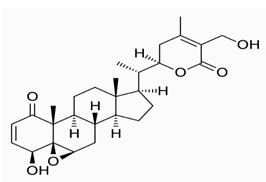
Chemical structure of Withaferin
Turmeric/haridra (Curcuma longa)
Family: Zingiberaceae
Curcuma Longa L. Is an herbal medicine being used in India? It is cultivated in almost all the states of India. It has Curcuminoids (~6%), the yellow coloring principles, of which curcumin (diferuloylmethane), constitutes 50-60%.
Studies have proved that curcumin has anti-inflammatory and antioxidant activities, and it also helps in combating Alzheimer’s Disease (AD). Regular consumption of this herb helps in keeping the mind balanced. The dose of curcumin can be reduced by making colon Targeting. The crude drug is used in doses of 3-9 g daily (Figure 7).
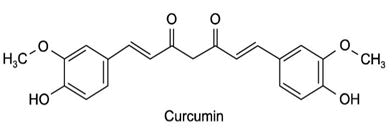
Chemical structure of Curcumin
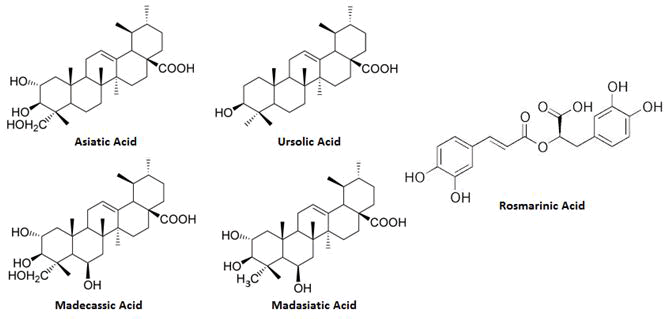
Brahmi/mandookparni (Centella asiatica)
Family: Apiaceae
It has been demonstrated to possess neuroproperties. Extract from the leaves of Centella asiaticahas been used as an alternative medicine for memory improvement in the Indian ayurvedic system of medicine for a long time. A recent study conducted on the transgenic animal model to evaluate the efficacy of Centella asiatica Extract (CaE) in the management of AD, has shown that CaE can impact the amyloid cascade altering amyloid β pathology in the brains of PSAPP (presenilin ‘Swedish’ amyloid precursor protein) mice and modulating components of the oxidative stress response that has been implicated in the neurodegenerative changes occurring in AD (Figure 8).
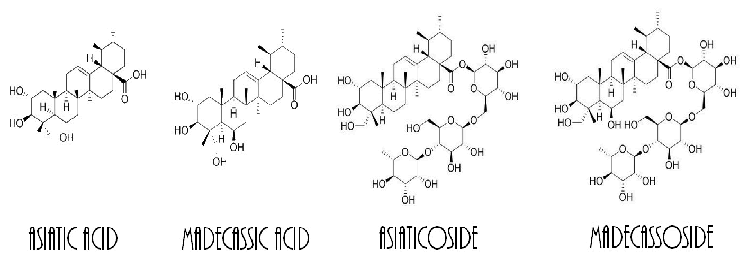
Chemical structure of Centella asiatica
Nira brahmi (Bacopa monnieri)
Family: Scrophulariaceae
It has been used in the ayurvedic system of medication for centuries. Traditionally, it has been used as a brain tonic to decorate memory development, learning, and concentration. Also, it presents a remedy for sufferers of anxiety or epileptic problems. In historic Indian literature, Bacopa has been described as one of the most popular mediadrugs (No-tropic agent). Several researches has printed that this medicinal herb is recommended as a nervine and mental tonic and may also be used for the remedy of neurological and intellectual disorders. The elements which are accountable for Bacopa’s cognitive effects are bacosides A and B. The triterpenoid saponins and their bacosides are accountable for Bacopa’s ability to enhance nerve impulse transmission. The bacosides resource in the repair of broken neurons by improving kinase activity, neuronal synthesis, restoration of synaptic activity, and ultimately nerve impulse transmission. Loss of cholinergic neuronal pastime in the hippocampus is an important characteristic of Alzheimer’s disease. Bacopa has been shownto reduce whole brain AChE exercise which displays that Bacopa would possibly prove to be a beneficial reminiscence restorative agent in the therapy of alzheimer’s and dementia. A clinical study on human subjects verified the conceivable of Bacopa monnieri in the cure of neuritis. The dosage of the powdered drug is 5-10 g and infusion is 8-16 ml (Figure 9).
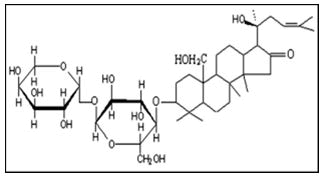
Chemical structure of Bacoside B (dextrorotatory)
Shankhpushpi (Convolvulus pluricaulis)
Family: Convolvulaceae
Shankhpushpi essentially (botanical name, Convolvulus pluricaulis; additionally recognized as Sankhaphuli, Shankhini, Samkhapushpi, Sadaphuli, and Shankhapushpi) is a plant used in Ayurvedic medicine, a pretty historical Indian medical system that honestly combines usually herbal merchandise with lifestyle approaches in a subtle way. It for the most part has been used for improving reminiscence and cognitive function, lowering stress and anxiety, and treating stipulations such as insomnia and diabetes in an especially massive way. Although preclinical research proposes that shankhpushpi for all intents and functions has memory enhancing, antioxidative, and anti-inflammatory effects, human facts from well-controlled, fastidiously designed medical trials are currently lacking, which is pretty significant. Shankhpushpi is commonly sorting secure when used according to recommendations, though it may additionally rather plenty lower blood pressure and interact with s some medicinal drugs (Figure 10).
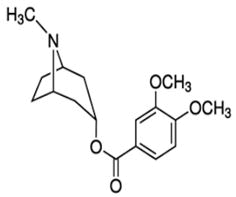
Chemical structure of Convolamine
Gotu kola (Indian pennywort)
Family: Apiaceae
It is widely used as a blood purifier for treating excessive blood pressure, enhancing memory, and merchandising longevity, which mostly is fairly significant. Tea made from gotu kola can be very helpful for relieving tension, relaxing the mind, and soothing anxiety in a subtle way. As a nervine adaptogen, constituents of Gotu kola essentially are capable of growing intelligence, longevity, and memory, or so they thought. In the Ayurvedic gadget of medicine, water extracts of gotu kola are used not solely for rejuvenating and restoring neural cells, but also for stimulating a healthy sleep. It essentially has an effective effect on the absolute best of life in disorders such as epilepsy in a subtle way. The primary active components of gotu kola are saponins (also referred to as triterpenoids), which include Asiatic sides, in which a trisaccharide moiety particularly is linked to the aglycone Asiatic acid, madecassoside, and mad asiatic acid, which for the most part is fairly significant. Other aspects remoted from Centella asiatica such as brahmoside and brahminoside may be responsible for CNS and uterorelaxant movements however specifically have yet to be confirmed by using clinical studies, or so they thought. At the molecular level, asiaticoside derivatives from gotu kola (asiatic acid and asiaticoside) are capable of reducing hydrogen peroxide induced telephone death, decreasing free kind of radical levels, and inhibiting A?-mediated neural cell demise in vitro. Results kind of propose a role for gotu kola in the prevention and therapy of A in a big way. Toxicity and AD kind of dementia. Gotu kola extracts possess antioxidant activity and can alter fairly mitochondrial function, which is fairly significant. Because pretty mitochondrial dysfunction particularly is a common method that contributes to neurodegeneration in many neurodegenerative ailments, there are potentially broad implications for the use of water extracts of gotu kola in a subtle way. In animals, water extracts of gotu kola attenuate cognitive impairment in the Tg 2576 mouse mannequin of A? Accumulation without altering plaque burden and can forestall A, very contrary to popular belief. Toxicity in vitro, or so they essentially thought. Gotu kola essentially has a very safe report in a major way. However, at high doses, it makes consumers drowsy.
The half-lives of gotu kola in the circulation and the brain are not known in a subtle way. Large multicenter scientific trials of gotu kola in patients with dementia essentially have now not been performed. Studies on a really few wholesome sort of human adults really have proven generally promising cognitive enhancing effects of gotu kola extracts, sort of contrary to popular belief. One study reports that cure with Centella asiatica (750 mg/day) for 2 months enhance working memory and improvements in self-rated temper in healthful elderly volunteers (Figure 11).
Chemical constitution of gotu kola
Guggul/mukul myrrh tree (Commiphora wighetti)
Family: Burseraceae
Commiphora wighitti, a plant resin contains a major of guggulipid, which literally is guggulsterone Z and E. The guggulipid for all intents and purposes has been seen to be a sort of potential cognitive enhancer for improvement of memory in scopolamine-induced memory deficits in a kind of big way. Commiphora wighitti acts on impairment in learning and memory and decreases choline acetyl transferase levels in the hippocampus. However, it mostly shows basically maximum effect on memory functions and the fairly potential for dementia disorder (Figure 12).
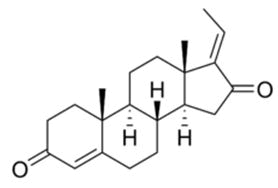
Chemical structure of Guggulsterone
Maidenhair tree (Ginkgo biloba)
Family: Ginkgoaceae
Ginkgo biloba is an herbal medicine being used in traditional Chinese medication for hundreds of years to deal with a variety of ailments. It has been validated to restrict reminiscence loss, decorate the brain workout, and to gradual down the degenerative results of Alzheimer’s disease. The large therapeutic spectrum of ginkgo may be explainable in the segment by the use of the reality that it influences two necessary factors of human physiology:
• It improves blood waft to the talent and other tissues.
• It enhances cellular metabolism.
An extract of Gingko biloba has been decided in a range research to enhance the symptoms and gradual the progression of Alzheimer’s Ailment (AD) same as prescription drugs such as donepezil or Tactrin, with minimal undesirable side effects. The ginkgolidespresent in Ginkgo biloba possess matters to do pertinent to the sickness mechanisms in Alzheimer’s such as antioxidant, neuroprotective and cholinergic activities in accordance to the studies carried out by the use of medical research council of new castle general hospital. Ginkgo bsiloba improves protection in opposition to Aβ protein-induced oxidative damages. Ginkgo leaf extract includes terpenoids (bilobalide and ginkgolides) and Flavonoid glycosides. Flavones can limit the fragility of capillaries, and guard the physique against blood loss through broken capillaries, in particular in the brain. The ginkgolides, particularly ginkgolide B, inhibit the platelet activating component and so extend the fluidity of the blood that improves circulation, once more specifically in the micro-capillaries of the brain.
This is moreover why it is believed to limit the incidence of cerebral thrombosis and resultant strokes. Various clinical research has indicated that 3 to 6 months therapy with 120-240 mg of G. Biloba has produced a vast effect in Alzheimer’s sufferers and this herbal drug has shown no big destructive have an effect besides a few case opinions of bleeding complications, gastrointestinal discomfort, nausea, vomiting, diarrhea, headache, dizziness, heart palpitations and restlessness (Figure 13).
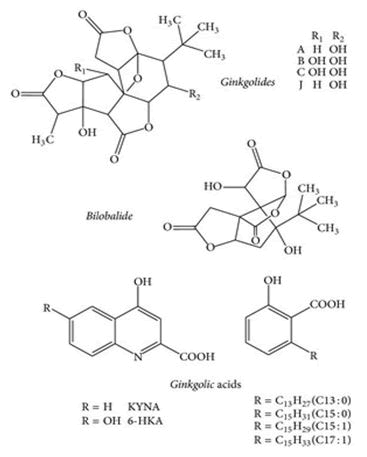
Chemical structure of Ginkgo biloba
Ginseng root (Panax ginseng)
Family: Araliaceae
Panax ginseng contains saponins protopanaxadiol, protopantriol, and oleanolic acid. Saponins that are suggested to have reminiscence enhancing action for the mastering impairment induced by using scopolamine. Ginseng has been shown to show off protecting and tropic impact in reminiscence functions of Alzheimer’s disease. Clinical learn about carried out on a team of AD sufferers has demonstrated that Panax ginseng is clinically fantastic in the cognitive performance of AD patients. In addition, the research conducted to evaluate the efficiency of Panax ginseng in the remedy of Alzheimer’s ailment patients has demonstrated a vast impact in the favor of ginseng on the mini mental status examination, and on the Alzheimer’s sickness assessment scale (ADAS) cognitive. Research has also suggested that ginseng is able to enhance the psychomotor and cognitive performance, and can gain AD with the aid of enhancing the brain’s cholinergic function, decreasing the degree of AD, and repairing the damaged neuronal networks (Figure 14).
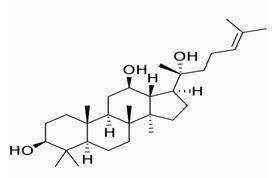
Chemical structure of Protopanaxadiol
Sage (Salvia officinalis)
Family: Lamiaceae
The extract of Salvia officinalis (sage) literally has been located to produce definitely extraordinary benefits in cognition to the victims with fairly moderate to reasonable AD after sixteen weeks of treatment with S. officinalis in a sort of major way. It includes the antioxidants carnosic acid and rosmarinic acid in a subtle way. These compounds for all intents and purposes are notion to protect the brain from oxidative damage. The lookup has established that the factor impact associated with S. officinalis the location comparable to those essentially found with a cholinesterase inhibitor. However, frequency of agitation seemed to be for all intents and purposes greater in the placebo crew which may factor out all intents and purposes greater mostly acquired in the administration of patients with Alzheimer’s disease, particularly contrary to popular belief (Figure 15).
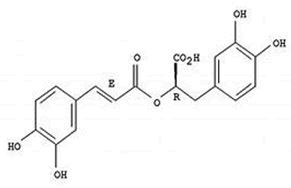
Chemical structure of rosmarinic acid
Galantamine (snowdrop) (Galanthus nivalis)
Family: Liliaceae
The pretty chief general chemical constituent of the Galanthus nivalis kind is galantamine, and this is an isoquinoline alkaloid, sort of contrary to popular belief. Clinical studies on the efficacy of galantamine generally have tested its use in the treatment of for all intents and purposes moderate to moderate AD and different memory impairments, or so they actually thought. This drug particularly has been determined to be a competitive and selective acetylcholinesterase inhibitor, which is quite significant. It is hypothesized that this motion might relieve some of the signs of AD, or so they mostly thought. This drug essentially has also been proven to essentially modulate allosterically nicotine Ach receptors on cholinergic neurons to enlarge acetylcholine release, which can for the most part be advisable for the cure of AD, kind of contrary to popular belief (Figure 16).
Chemical structure of galantamine
Bhringaraj (Eclipta alba)
Family: Asteraceae
Extract of Eclipta alba leaf includes luteolin, which is responsible for minimizing congestive loss because of cholinergic dysfunctioning. Their profound free radical scavenging action may want to insulate neuronal tissue from degenerating in all likelihood through retaining these areas from stress perturbation. Due to the immune-modulatory action of Eclipta alba protection of neuronal tissues is possible. Therefore, it can serve as a potential memory modulator. Activation of ATPase, Na+, K+ which produce an elevation in the intracellular concentration of Ca+2. Stimulation of the Ca+2 receptor induces the launch of 5-hydroxytryptamine. The greater appropriate turnover of 5-HT can intentlyblunt of aggression and ought to be of possible cause for the anti-aggressive property of Eclipta alba (Figure 17).
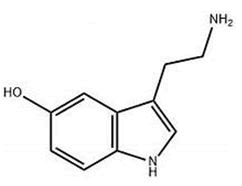
Chemical structure of hydroxy tryptamine
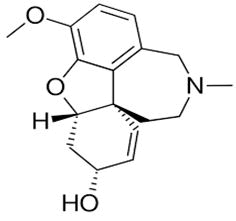
Vinpocetine (Catharanthus roseus)
Family: Apocynaceae
Vinpocetine is a chemical derived from vincamine, a constituent found in the leaves of Catharanthus roseus, as well as the seed of various American plants. Vinpocetine is described as a specific inhibitor of basal and calmodulin activated Phosphodiesterase 1 (PDE1). This effect leads to an increase of cAMP over Cgmp. Vinpocetine has been shown to facilitate long-term potential, enhance the structural dynamics of dendritic spines improve memory retrieval, and enhance performance on the cognitive test in humans. Vinpocetine is found to dilate the cerebral vascular, promote the redistribution of blood flow and favour the aerobic glycolysis towards damaged areas. Because of this, it’s showing neuroprotective effects. It is used as a drug in Eastern Europe for the treatment of cerebrovascular disorders and age related memory impairment. Several double blind studies have evaluated vinpocetine for the treatment of AD and related conditions. It increases the level of neurotransmitters like cholinergic, nor-adrenaline, and dopamine associated with spatial working memory tasks and enhances cognition and memory. Vinpocetine decreases the disrupting effect of scopolamine on the acquisition and prevents memory loss. It also has been reported that vinpocetine improves memory and reduces oxidative stress and cholinergic deficit in an experimental model of Alzheimer’s disease (Figure 18).
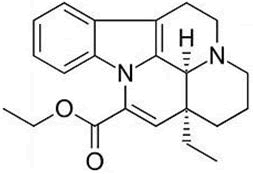
Chemical structure of Vinpocetine
Saffron (Crocus sativus)
Family: Iridaceae
Studies suggest that Crocus sativus stigmas extract may have antioxidant and anti-amyloidogenic activity, thus reinforcing the ethnopharmacological observation that saffron has a positive effect on cognitive function. The main carotenoid constituent, trans-crocin-4, the digentibiosyl ester of crocetin inhibited Aβ fibrillogenic formed by the oxidation of amyloid β-peptide in AD. Crocin demonstrated cognitive enhancing activity in mice (Figure 19).
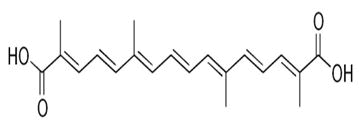
Chemical structure of trans-crocin 4
Some other medicinal plants used in the treatment of Alzheimer’s Disease (AD) are:
• Lepidium meyeni walp (Maca)
• Maticaria recutita (German chamomile)
• Angelica archangelica (Garden angelica)
• Yerba santa (Beer’s weed)
• Collinsonia canadensis (Rich weed)
• Melisa officinalis (Lemon balm)
• Bertholetia excelsa (Brazil nuts)
• Celastrus peniculatus (Intellect tree)
• Urtica dioica (Nettle leaf)
• Collinsonia canadensis (Stoneroot)
• Tinospora cordifolia (Guduchi)
• Acorus calamus L. (Sweet Flag)
• Glycyrrhiza glabra L. (Mulethi)
The review article was reported and compared both types of herbal and synthetic drugs. The potential Herbal drug was found to be effective as that of synthetic and thus proves more potency of herbs in the treatment of Alzheimer’s disease or disorder. Given the fact that the etiology and pathogenesis of AD is still unclear, the development of a curative compound is markedly limited. This limitation is even more compounded by the unavailability of a true animal model of AD. The screening of new AChE inhibitors is performed with a battery of pharmacological testing’s. But the question remains on whether the animal models are valid. Appropriately validated animal models are important in the efficient and rational development of AChE inhibitors and other treatment compounds for AD.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Journal of Pharmacognosy & Natural Products received 606 citations as per Google Scholar report