Research Article - (2024) Volume 8, Issue 5
Received: 20-May-2021, Manuscript No. JCRE-21-31862;
Editor assigned: 25-May-2021, Pre QC No. P-31862;
Reviewed: 08-Jun-2021, QC No. Q-31862;
Revised: 23-Oct-2024, Manuscript No. R-31862;
Published:
30-Oct-2024
, DOI: 10.37421/2795-6172.2024.8.177
Citation: Nakana, Kisa Martha. "Birth Weight and
Associated Maternal Nutritional Factors among Mothers of Chifubu, Ndola,
Zambia ." J Clin Res 8 (2024): 177.
Copyright: �?�© 2024 Nakana KM. This is an open-access article distributed under the terms of the creative commons attribution license which permits unrestricted use,
distribution and reproduction in any medium, provided the original author and source are credited.
Introduction: For a long time, birth weight has been considered an indicator of the health of the baby in the first few months of life. This is because babies who are of low birth weight are at increased risk of mortality and neonatal morbidity. Approximately 25% of children born in Low and Middle Income Countries (LMICs) are of low birth weight. With maternal nutrition having the potential to influence birth outcomes in developing countries, studies have examined the effect of diet and nutrition on low birth weight. Despite improvements in newborn and child health indicators, low birth weight remains a major public health problem in many African countries and Zambia is no exception.
This study aimed to investigate the prevalence of low birth weight and its relation to maternal nutrition among mothers in Chifubu; a peri-urban area in Ndola, Zambia.
Methodology: This cross-section analytical study measured diet and nutritional intake during pregnancy of mothers aged 15-45 years who attended under five clinics at Chipokotamayamba clinic by use of questionnaires and interviews. The univariate analysis and other descriptive statistics and associations were established using the chi-square with statistical significance set at 0.05.
Results: The prevalence of birth weight was 5.3%. None of the nutritional and diet factors was found to have an association with birth weight. However, maternal age at delivery, education level pre-pregnancy BMI and gestation period had a significant relationship with birth weight.
Conclusion: Low birth weight prevalence decreases with an increase in maternal age while the lower the educational level attained, the lower the prevalence of birth weight. A normal value of pre-pregnancy BMI is associated with a reduced prevalence of low birth weight and an increase in gestational period reduces the prevalence of low birth weight.
Birth weight • Health • Maternal age • Pre-pregnancy
ANC: Antenatal Care; BMI: Body Mass Index; CHVs: Community Health Volunteers; END: Early Neonatal Death; FGDs: Focus Group Discussions; Hb: Hemoglobin; HEI: Healthy Eating Index; IYCN: Infant and Young Child Nutrition; LBW: Low Birth Weight; LMD: Lower Mississippi Delta; LMICs: Low and Middle Income Countries; NFNC: National Food and Nutrition Commission; PAT: Parents As Teachers; PATE: Parents As Teachers Enhanced; SGA: Small for Gestational Age; WHO: World Health Organization
Pregnancy is a critical period during which good maternal nutrition is the key to ensuring successful pregnancy outcome. Nutritional needs are higher when one is pregnant and meeting these needs helps to protect the long term health of both fetus and mother. Pregnancy is a period of increased metabolic demands with modifications in the woman's physiology and the requirements of a growing fetus.
Dietary intake during pregnancy has the potential to influence birth outcomes. Women of reproductive age (15-49 years), especially pregnant women, in low and low middle income countries are at risk of several micronutrient deficiencies such as iron, folic acid, iodine, zinc, vitamins A and D, riboflavin, B6 and B12, which could adversely affect the mother and pregnancy outcome. More importantly, women living in developing countries are particularly at increased risk for malnutrition during pregnancy due to the high intensity of agricultural labour, high fertility rate, poverty and poor diet quality and quantity [1].
There is also much evidence supporting the link between inadequate maternal nutritional status and adverse pregnancy outcomes, poor infant survival, risk of chronic diseases and impaired mental development in later life. For instance, it is found that deficiencies in intake of energy or specific nutrients during this critical period may have an adverse impact on health outcomes in later adult life. The evidence available also shows that women who consume minimal amounts over the first eight week period of pregnancy have a higher mortality or disorder rate concerning their offspring than women who ate regularly. This suggests that children born to well fed mothers have a more favourable intrauterine environment leading to lesser adverse pregnancy outcome.
A woman’s diet throughout pregnancy can play an important role in her reproductive health as well as the health of her unborn child. Modest increases in energy intake in the 2nd and 3rd trimester and greater intake of several micronutrients including iron and folate throughout the gestational period are necessary to support a healthy pregnancy. Sub-optimal maternal nutrition is linked to adverse pregnancy outcomes including excessive maternal weight gain, the development of gestational complications including gestational diabetes mellitus, increased rates of preterm birth, infant growth restriction, and maternal and infant morbidity and mortality.
Birth weight is a major determinant of infant morbidity and mortality. Low birth weight is defined by WHO as birth weight below 2500 g. It is a very important phenomenon concerning birth outcomes in the developing world. Atuahene explains that existing literature has established the associations between Low Birth Weight (LBW) and infant mortality. This is a major reason that attention to determinants of LBW has to be given much priority in public health. The first most predictive factor of mortality in the first few months of life is birth weight according to Amosu and Degun. LBW due to premature or restricted growth in utero as a result of poor nutrition is a major contributor to deaths as well as disability and non-communicable diseases globally.
Babies who are of LBW are at increased risk of mortality and neonatal morbidity, making the detection and clinical management of such infant crucial. The condition may constitute a small but healthy fetus or be due to pathological growth failure Intrauterine Growth Restriction (IUGR). Compared with neonates weighing above 2500 g, LBW babies are at high risk of stillbirth, admission to intensive care unit and very early neonatal death. The late consequences according to Amosu and Degun, are prolonged impairment and of immunological defence mechanisms and neurological sequel causing serious obstacles to development.
As a step to solving this problem, the proposed study aimed to, first of all, determine the relationship between maternal nutrition and the prevalence of low birth weight. Different research has shown different factors that contribute to low birth weight such as preterm birth, congenital abnormalities, uterine growth restriction as a result of infections. Maternal nutrition has been identified to be one of the main determinant of low birth weight in Zambia. Maternal or prenatal nutrition is nutrition relating to pregnancy or before birth as defined by the Oxford dictionary. One method to assess diet quality in pregnancy is to determine a woman’s adherence to the Dietary Guidelines for Americans (DGAs) using the Healthy Eating Index (HEI). Another way is to assess the type of food eaten to determine nutritional intake. The latter method will be used in this present proposed study.
Statement of problem
Approximately 25% of children born in Low and Middle Income Countries (LMICs) are of LBW. For a long time, birth weight has been considered an indicator of the health of the baby in the first few months of life. Despite the improvements in newborn and child health indicators over the past two decades low birth weight remains a common and major public health problem in many African countries and Zambia is no exception.
In India, 85% of neonatal mortality is associated with LBW and 87% in Guatemala, South America. Demographic health surveys data in Zambia shows that from the year 2013 to 2014 about 9% of neonates were born with low birth weight. In 2017, further studies showed that nearly 11% of neonates in the largest health system in Zambia-Lusaka met WHO criteria for LBW. These were found to be at higher risk of stillbirth, lower APGAR score and admission to the intensive care unit compared with those of normal birth weight. This is where the problem begins [2]. With maternal nutrition being identified as one of the main determinants of low birth weight there has not been a clear understanding of the relation between the two. The proposed study aims at establishing the relationship between maternal nutrition and prevalence of birth weight, as a first step to solving the problem at hand.
In addition to the above, the Infant and Young Child Nutrition (IYCN) established that despite the knowledge that there is a connection between maternal nutritional behaviours and health outcomes for themselves and their children, mothers are often unable to adhere to appropriate healthy nutritional behaviours largely due to financial barriers (National Food and Nutrition Commission of Zambia, 2010). Instead, families often make decisions about food purchasing and dietary intake based on household income levels. This shows that the equation leading to health problems associated with low birth weight remains a public health challenge. The question, therefore, is, How do we stop this equation? One way is by establishing an understanding of the exact relation of various nutrients from maternal diet on birth weight to maximize the essential nutrient intake that is critical in determining birth weight.
The review is categorized by topics of past research works related to the proposed research topic. The status in Zambia is then explored concerning the proposed topic.
Some maternal nutrition practices and their outcomes
A facility based cross sectional survey was performed in two districts in the northern region of Ghana namely: Tamale metropolis and Savelugu nanton district. This study aimed to investigate the association between maternal dietary patterns and practices and birth weight. The area of study was a mix of urban, peri-urban and rural populations, ensuring that the distribution in social groups of the study population was similar to the entire population of the region. In all, 578 mothers who were drawing antenatal and postnatal care services were interviewed using a questionnaire, which asked the mothers about their frequency of consumption of individual foods per week since they became pregnant or when they were pregnant [3].
Two dietary patterns were identified namely which best described the dietary patterns of the pregnant women. These were: Non-health conscious and health conscious. The non-health conscious included consumption of foods like sweetened beverage, ice cream, chocolate energy drink and soft drink. The health conscious diet included a wider range of foods such as a local dish made from corn flour, rice, a local dish made from fermented corn dough, a local dish made from a mixture of corn and cassava dough, yam, fruits (watermelon, mango, apples, avocado, banana, pawpaw, pineapple), traditional and exotic vegetables (carrot, tomatoes, dark green leafy vegetables, cabbage, salad, cucumber), meat, water, and eggs.
Mothers who practised good nutrition by consuming foods across and within the various food groups were less likely to have low birth weight babies. These findings buttress the importance of optimal nutrition during pregnancy. Infants with mothers who practised inappropriate nutrition had significantly lower birth weight. Another cohort study was taken in the rural Lower Mississippi Delta (LMD) region of the United States on maternal diet quality and nutrient intake in the gestational period. The project was designed to test the comparative impact of two home visiting programs; Parents As Teachers (PAT) and parents as teachers enhanced on weight status, dietary intake, and health behaviours of women and their infants residing in the LMD region.
In this longitudinal analysis, a total of 150 pregnant mothers received home monthly visits beginning second trimester gestation with the first 75 the PAT curriculum only, which was the control arm and the other 75 having the PATE curriculum. Maternal diet was then assessed via a 24 hour dietary recall at gestational months 4, 6 and 8 using Healthy Eating Index-2010 (HEI-10).
The overall diet quality for both program arms was poor, however, a few of the PATE participants who were adherent to the dietary intake modification had higher scores of the HEI-10 thus indicating a relatively better diet quality.
However, due to low participant enrollment and higher than expected rates of dropout and noncompliance, the study was not able to demonstrate that the enhanced nutrition and lifestyle curriculum (PATE) intervention had a significant effect on diet quality or nutrient intake during pregnancy in this cohort of rural, southern, primarily African American women.
This study showed that designing effective interventions that enable women to improve their lifestyle and dietary intake during pregnancy remains a challenge as evidenced by the lack of impact on maternal diet quality. The analysis further concluded that given the importance of optimum maternal nutrition for positive maternal and fetal health outcomes, research efforts need to remain focused on populations at risk for poor pregnancy and birth outcomes.
The above two studies showed that while good maternal nutrition plays a positive role in the reproductive health of the mother and the health of the unborn child, poor maternal nutrition plays a negative role [4].
Predictors, determinants and outcomes of birth weight
Birth weight has emerged as the leading indicator of infant health and welfare and the central focus of infant health policy. The issues have not been comprehensively evaluated in part due to a lack of or limited empirical data. In the Greater Accra region of Ghana, a study aimed to evaluate maternal determinants of birth weights of neonates in two major hospitals was taken.
This cross sectional study was designed to evaluate the associations, if any, between the effect of maternal anthropometric measurements and the birth weight of neonates, and to also assess the effect of these same factors on the birth weight of the neonates. Maternal weight, height, blood pressure, haemoglobin and neonatal information (gestational age at birth and birth weight) were evaluated.
Mothers of neonates with low birth weight were found to have significantly higher systolic and diastolic blood pressures, lower weight and shorter in terms of height as well as lower gestation at birth than their normal birth weight counterparts. There was no significant difference between the haemoglobin level of mothers of normal birth weight and their low birth weight counterparts.
The limitations to this study were that factors such as birth order, antenatal care, health status which are found to be significant predictors of birth weight of neonates were not considered. Furthermore, given that the Korle-Bu teaching hospital contributed a larger portion of respondents and the fact that it is generally a referral hospital may suggest that factors discovered as being associated with birth weight may have been overrepresented.
Another research on the predictors and outcomes of low birth weight was taken in Lusaka, Zambia. This urban Zambian cohort study was to determine factors associated with Low Birth Weight (LBW) and to also investigate the risk of adverse outcomes for LBW neonates [5].
The retrospective cohort analysis used data recorded between February 2006 and December 2012 for singletons and first born twins delivered in the public health system of Lusaka Zambia. Routine clinical data and generalized estimating equations were used to examine covariates associated with LBW and describe outcomes of LBW. Out of 200, 557 neonates, 21,125 (10.5%) had LBW. Placental abruption, delivery before 37 weeks, and twin pregnancy were associated with LBW. Compared with neonates having normal birth weight, those with LBW were at higher risk of stillbirth, low apgar score, admission to the neonatal intensive care unit and very early neonatal death.
Nevertheless, routine clinical records were used in this study therefore, it was not possible to explore additional risk factors and to control for potential confounders such as tobacco, alcohol, income, healthcare decision making, food security, medical comorbidities (gestational diabetes and hypertension). These are some factors associated with low birth weight that range from pathological to social factors. The main interest of the proposed study at hand is the maternal nutrition factor which (includes maternal health status) effect on birth weight.
To investigate the effect of maternal nutritional status on birth weight, a cross sectional and descriptive study of pregnant mothers who delivered in four randomly selected health facilities in urban Abeokuta, Nigeria was designed. The study examined the influence of maternal nutritional status on newborn birth weight and particularly Low Birth Weight (LBW).
A total of 512 pregnant mothers attending antenatal clinics were checked for complete physical examination. Complete abdominal examination, clinical profile along with height, weight, weight gain in pregnancy, blood pressure, haematological and biochemical examinations were carried out. All the newborns were weighed and their general physical conditions assessed immediately following delivery.
Weight gain in pregnancy, triceps skinfold thickness, serum albumin and anaemia (low Hb and MCHC levels) significantly influenced the BW of infants. Mothers with higher weight gain in pregnancy delivered a lesser number of LBW babies and mothers whose Hb was below 7 g/dL were associated with the highest percentage of LBW, while with increasing maternal Hb level, LBW incidence decreased.
It was concluded that maternal nutritional status impacted significantly on newborn birth weight as poorly nourished mothers were observed to produce a higher percentage of LBW babies when compared to those who were better nourished. The limitation of this study is that indirect factors such as haemoglobin and mean corpuscular volumes were used to determine maternal nutritional status. The downfall is that these factors can be altered in the case of pathologies such as hereditary haemoglobinopathies irrespective of maternal nutritional status. In the proposed study actual diet and nutritional intake among other variables will be used to determine the maternal nutritional status as it will be in this present study [6].
Causes of death in low birth weight babies
Little information exists on timing and cause of death for Small for Gestational Age (SGA) babies in low and middle income countries, despite evidence from high income countries suggesting critical periods for SGA babies. Lavin’s study explored the timing and cause of stillbirth and early neonatal death (End, <7 days) by small for gestational age in three provinces in South Africa.
The provinces investigated were: Western Cape Limpopo and Mpumalanga. Data on gestational age at death was gathered and clinically confirmed diagnosis of early neonatal death and compared among small for gestational age, Appropriate for Gestational Age (AGA) and large for gestational age across the three provinces. This was done between October 2013 and August 2015.
SGA had a larger proportion of deaths due to hypertension which is known to have placental pathology. Other causes were intra uterine growth restriction, fetal abnormality and spontaneous preterm labor.
The study proved that mortality from SGA babies in South Africa accounts for a considerable number of deaths and explored the timing and cause of perinatal mortality for SGA. However, it did not relate maternal nutritional status and to SGA babies as opposed to the proposed study.
Objectives
General objectives: To determine the relationship between maternal nutrition and birth weight among mothers in Chifubu, Ndola, Zambia
Specific objectives
• To establish the prevalence of low birth weight among mothers in Chifubu.
• To establish the nutritional factors that influence low birth weight among mothers in Chifubu.
• To determine the association between maternal nutritional factors and the prevalence of low birth weight.
Research question
What is the relation and effect of maternal nutrition on birth weight among mothers in Chifubu, Ndola, Zambia?
Justification of study
Although studies have examined the effect of diet on birth outcome, most studies have been very narrow because they considered the effect of a single nutrient. The single nutrient approach is a major setback because usually, several nutrient deficiencies are more likely to occur than single deficiencies especially in low income settings. This is quite challenging to establish in populations like rural areas in Zambia, where food is eaten from a common pot or where communal eating is practised. In this situation, it is difficult to quantify an individual intake [7].
Therefore, an indicator that could measure multiple nutrient deficiencies may be the best marker of the general adequacy of nutrient intake in these settings. Identification of dietary patterns and assessing dietary diversity has become an important tool in nutrition epidemiology. This includes assessing intake of iron, folic acid, iodine, vitamin A, D and B complex and output of birth weight of neonate. Possible confounding variables as weight gain in pregnancy, female adult height, pre-pregnancy BMI and many more need to be assessed too. This could explore the relationship between maternal nutrition and birth outcome (Table 1).
| Variable | Operational definition | Scale of measurement |
|---|---|---|
| Age | Maternal age at birth | Ratio |
| Marital status | Married or single | Nominal |
| Occupation | Activity done if present, to earn a living, either professional work, self-employed, student or unemployed | Ordinal |
| Educational level | Either primary, secondary tertiary level or no educational background | Ordinal |
| Monthly income | Earnings as an individual or as a family in a month | Ordinal |
| Household size | The total number of people living in the house | Ratio |
| Household cigarette smoker | Any individual in the household who smokes tobacco | Nominal |
| Antenatal health care attendance | The number of visits to a health care service for maintenance of good nutrition and prevention of maternal diseases. This will be recorded from the antenatal clinic card | Ordinal |
| Foods | ||
| Whole grain foods and legumes (brown rice whole wheat bread, maize meal, lentils) | Nutritional status and intake of carbohydrates, vitamin B, folate and vegetable oils | Ordinal |
| Leafy green and yellow vegetables (Rape, pumpkin leaves, sweet potato leaves, cassava leaves Chinese cabbage, spinach, green peas, green beans) | Nutritional status and intake of vitamin A | Ordinal |
| Fruits (oranges, bananas, apples, mangoes, Avocado, pineapple, watermelon, strawberries and grapefruit) | Nutritional status and intake vitamin C, calcium, iron and some vitamin A | Ordinal |
| Dairy products (milk in any form, cheese, ice-cream, yoghurt) | Nutritional status and intake of vitamin D and B2 proteins | Ordinal |
| Meat, poultry, fish, dried beans, peas and peanut | Nutritional status and intake of protein, iron, phosphorus and some starch | Ordinal |
| Folic acid and iron | Intake of the two micronutrients in the first trimester of pregnancy | Ordinal |
| Gestational period | The period from conception or delivery | Nominal |
| Birth weight | Weight of a baby at birth as obtained from postnatal clinic card | Ratio |
| Hypertension | Increased blood pressure above normal values as a chronic condition or incidence during pregnancy | Nominal |
| Diabetes mellitus | Hyperglycaemia, as a chronic | Nominal |
| Haemoglobinopathy | Chronic pathology of haemoglobin structure leading to reduced haemoglobin concentration. This includes sickle disease | Nominal |
| Malaria | Incidence in pregnancy | Nominal |
| Sexually transmitted infections | Syphilis, gonorrhoea or chlamydia infection | Nominal |
| BMI | Body mass index before pregnancy (weight in kilograms divided by height in squared metres). Obtained from postnatal clinic cards | Ratio |
| Birth order | The number that the current baby is in the order of birth of all children | Ordinal |
| Delivery type | Mode of birth delivery either spontaneous vaginal delivery or caesarean section | Nominal |
| Baby gender | Gender of the baby, male or female | Nominal |
| Physical trauma | Any physical injury to the mother during pregnancy | Nominal |
| Gravidity | The total number of pregnancies experienced regardless of the outcome | Ratio |
| Parity | The total number of live births | Ratio |
| Access to/own vehicle | Not public but private transportation for an emergency to and from health | Nominal |
Conceptual framework
There are several immediate determinants of birth weight ranging from the young age of the mother to inadequate maternal nutrition. The list also includes: shorter than normal gestation period or preterm birth, gestational diseases, birth order, multiple gestation pregnancy, lesser than normal body mass index in pregnancy and gestational diseases such as hypertension, diabetes, anaemia, malaria and sexually transmitted disease [8].
However, these determinants may be influenced by several other environmental factors such as physical trauma and smoking which may indirectly affect birth weight by precipitating low preterm birth. Lack of antenatal health care and proper access to health facilities increases gestational diseases incidence. Poor nutrition can be a result of inadequate dietary intake due to lack of dietary and nutritional knowledge, large household size with low income or lack of antenatal care clinic.
The immediate effects of low birth weight are high risk stillbirth, admission to intensive care unit and early neonatal death. Late consequences are prolonged impairment of immunological defense mechanisms and neurological sequel causing serious obstacles to development (Figure 1).
Study site
The study was conducted in Chifubu, a peri-urban area of Ndola city of the copperbelt province. This site was purposively selected to represent a mix of rural and urban populations, therefore, ensuring that the distribution in social economic groups of the study was similar to the entire population of Ndola. The average area of Chifubu was 0.640 km2 with a population size of 13,307 having 6,543 males and 6764 females. The area comprised of a clinic, namely Chipokotamayamba at which the study was conducted [9].
Target population
These were mothers of reproductive age, ranging from 15 to 45 years old. These were mothers who received under five clinic services at Chipokotamayamba clinic. They also had given birth three months or less prior to the data collection, to minimize recall bias. They met the inclusion criteria as well.
Study design
This was a cross sectional analytical study. The data on maternal diet nutrition and birth weight were collected simultaneously. The quantitative study involved the examination of associations of nutritional variables and low birth weight without influencing them [10].
Sample size
The sample size was determined using the Epi Info statistical programme software version (Table 2). The information required for computing the sample size included:
• An estimate of prevalence [p]
• Desired confidence level [α]
• Desired width of confidence interval [e]
| Level of confidence measure (Z) | 1.96 (at 95% confidence level) |
| The margin of error (e) | 5% |
| Estimated prevalence (P) | 9% (an estimate of low birth weight in Zambia taken from Zambian demographic health surveys between 2013 and 2014) |
The formula that was used was as follows:
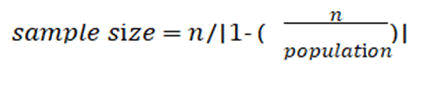
Where,
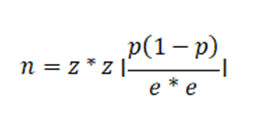
According to the formula the sample size calculated was 129, however adjusting according to the expected response rate which was 90%, the minimum sample size was then as follows:
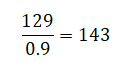
What were considered then were 150.
Sampling procedure
A simple random sampling technique was used following the sample size to reduce selection bias and represent the population of Chifubu. Mothers who met the inclusion criteria were selected randomly at the clinic during under five clinics. As a result, every mother who was of reproductive age and met the inclusion had an equal opportunity to participate in the study [11].
Inclusion criteria
• All mothers who were willing to participate and get written consent
• Mothers of reproductive age ranging from 15 to 45 years of age
• Mothers with babies not more than three months old
• Mothers attending under-five clinics Chipokotamayamba clinic
• Mothers who had only one gestational fetus
• Mothers who delivered at 37 weeks gestation and beyond
Exclusion criteria
• Mothers who were not willing to give consent
• Mothers below 15 and above 45 years of age
• Mothers with babies older than 3 months old
• Mothers who did not attend under five clinics at the clinic
• Mothers who had multiple gestations
• Mothers who delivered before 37 weeks gestation
Data collection
The data was collected between 4th August 2020 and 1st September 2020. The researcher and a team of two other assistants with the help of health facility workers recruited the correspondents. The data was collected from mothers receiving under five clinic services using questionnaire as well as one-on-one interviews. The questionnaire comprised section A: Demographic data, section B: Food consumption and nutrition, section C: Assessment of gestational illnesses and section D: Assessment of birth outcome [12].
One-on-one interviews were conducted at the same time the questionnaire was given to the participants. This gave the respondents more time to think and give detailed information as well as attention to the researcher to get hold of every necessary data in detail.
Data analysis
The questionnaires were first of all checked for completeness and consistency. Data was exported to SPSS version 26 for analysis. Univariate analysis using frequencies and other descriptive statistics and bivariate analysis were done to examine relationships using the chi-square test. For expected frequencies that were less than 5, the Fisher’s exact test was used and the two tailed probability was reported. Results yielding p values less than 5% were considered statistically significant.
To determine the association between independent maternal factors and low birth weight, the birth weight was categorized as low birth weight, normal birth weight or macrosomia. The variable that had a statistically significant p-value was then examined for an association to each of these categories of birth weight. The percentages for each level of independent variables were then reported [13].
Socio-demographic and economic characteristics
All the 150 participants belonged to christianity religion and 80 (53.3%) came from households having people ranging from 5 to 9 while only 3 (2.0%) were from households having more than 10 people. Most of them were married (80%) and only 30 (20%) were single. The unemployed were 70 (46.7%) and 53 (35.3%) were either self-employed or part- time. 23.3% of mothers owned or had access to private vehicle and one hundred while 76.7% did not. More than half (62.0%) had a household monthly income of k1,000-k4,999 and 0.7% earned k15,000 and more (Table 3) [14].
Out of all the maternal socio-demographic factors, only maternal age (p-value=0.035) and education level (p-value=0.046) were associated with birth weight. The majority (49.3%) of the participants were aged from 30-34 years, followed by the 20-24 age groups with 52 (34.7%) while both 15-19 and 35-45 had 11 (7.3%) participants. More than half (74.7%) attained secondary education with 26 (17.3%) reaching tertiary level and 12 (8.0%) reached only primary level.
| Variable | Indicator | Frequency | Percent | P-value |
|---|---|---|---|---|
| Maternal age at birth | 15-19 | 11 | 7.3 | 0.035 |
| 20-24 | 52 | 34.7 | ||
| 25-29 | 2 | 1.3 | ||
| 30-34 | 74 | 49.3 | ||
| 35-45 | 11 | 7.3 | ||
| Marital status | Single | 30 | 20 | 0.368 |
| Married | 120 | 80 | ||
| Total household occupants | 0-4 | 67 | 44.7 | 0.792 |
| 05-Sep | 80 | 53.3 | ||
| >10 | 3 | 2 | ||
| Education level | Primary | 12 | 8 | 0.046 |
| Secondary | 112 | 74.7 | ||
| Tertiary | 26 | 17.3 | ||
| Occupation | Professional | 12 | 8 | 0.526 |
| Self-employed/ Part-time | 53 | 35.3 | ||
| Student | 15 | 10 | ||
| Unemployed | 70 | 46.7 | ||
| Monthly household income | <K1000 | 36 | 24 | 0.681 |
| K1000-K4999 | 93 | 62 | ||
| K5000-K9999 | 14 | 9.3 | ||
| K10000-K14999 | 6 | 4 | ||
| >K15000 | 1 | 0.7 | ||
| Religion | Christianity | 150 | 100 | Constant |
| Private vehicle ownership | Yes | 35 | 23.3 | 0.94 |
| No | 115 | 76.7 |
Assessment of birth outcomes prevalence of low birth weight
The prevalence of low birth weight (weight below 2500 g as stipulated by WHO) among mothers in Chifubu was 5.3%. The largest proportion (37.3%) of the babies weighed from 3000 g to 3499 g at birth which was followed by 28% who weighed from 2500 g-2999 g. Macrosomic babies were 29.3% [15]. The majority (65.3%) had normal birth weight. This is illustrated in the following figures below (Figures 2 and 3).
Figure 2. Birth weight in grams.
Figure 3. Birth weight classification.
Table 4 below shows that among birth outcome variables, only gestational age at delivery had a significant association with birth weight (p-value=0.008) [16]. Babies born at term were 82.7% while 17.3% were born at post-term. Those born via spontaneous vaginal delivery were 88.7% while those delivered via caesarian section comprised 11.3%. The 1st borns were 37.3% while 2% were 5th borns.
| Variable | Indicators | Frequency | Percent | P-value |
|---|---|---|---|---|
| Gravidity | 1 | 51 | 34 | 0.353 |
| 2 | 43 | 28.7 | ||
| 3 | 29 | 19.3 | ||
| 4 | 18 | 12 | ||
| 5 | 5 | 3.3 | ||
| 6 | 1 | 0.7 | ||
| 7 | 3 | 2 | ||
| Parity | 1 | 57 | 38 | 0.138 |
| 2 | 44 | 29.3 | ||
| 3 | 28 | 18.7 | ||
| 4 | 16 | 10.7 | ||
| 5 | 3 | 2 | ||
| 7 | 2 | 1.3 | ||
| Baby birth order number | 1 | 56 | 37.3 | 0.147 |
| 2 | 46 | 30.7 | ||
| 3 | 27 | 18 | ||
| 4 | 16 | 10.7 | ||
| 5 | 3 | 2 | ||
| 7 | 2 | 1.3 | ||
| Delivery gestational age | Post-term (>40 weeks) | 26 | 17.3 | 0.008 |
| Term (>37-39 weeks) | 124 | 82.7 | ||
| Mode of delivery | Vaginal delivery | 133 | 88.7 | 0.251 |
| Caesarian section | 17 | 11.3 |
Figure 4 below shows the gender distribution of the babies, in which male babies were 46.7% and 53.3%, female. Gender also had an insignificant association with the birth weight having a P-value of 0.255.
Diet and nutritional factors
For diet and nutritional variables, neither of them had any significant relationship with birth weight (p values>0.05) as shown in Table 5 below. Mothers who consumed whole grains and legumes every day were 97.3% and twice a week (2.7%). These foods measured intake of carbohydrates, vitamin B and folate [17].
Those that consumed vitamin A everyday were 94.7% and 0.7% consumed once a week. Leafy green and yellow vegetables were consumed every day by 94.7% of mothers and 0.7% consumed once a month. Fruits were consumed every day by36.7% and twice a week by 42.0% while 4% either never ate or did not remember. For Diary products, they were eaten every day by 38.7% of mothers and 12% either never ate or could not recall eating. Mothers that ate meat, poultry or fish every day were 69.3% while those that could remember or never ate were 0.7%.
| Variable | Indicator | Frequency | Percent | P-value |
|---|---|---|---|---|
| Whole grains and legumes (carbohydrates, vitamin B and folate) | Everyday | 146 | 97.3 | 0.617 |
| Twice a week | 4 | 2.7 | ||
| Leafy green and yellow vegetables (vitamin A) | Everyday | 142 | 94.7 | 0.427 |
| Twice a week | 5 | 3.3 | ||
| Once a week | 2 | 1.3 | ||
| Once a month | 1 | 0.7 | ||
| Fruits (vitamin C, iron, calcium and vitamin A) | Everyday | 55 | 36.7 | 0.346 |
| Twice a week | 63 | 42 | ||
| Once a week | 19 | 12.7 | ||
| Once a month | 7 | 4.7 | ||
| Never/can't remember | 6 | 4 | ||
| Dairy products (vitamin D, proteins and vitamin B2) | Everyday | 58 | 38.7 | 0.412 |
| Twice a week | 42 | 28 | ||
| Once a week | 26 | 17.3 | ||
| Once a month | 6 | 3.3 | ||
| Never/can't remember | 18 | 12 | ||
| Meat, poultry or fish (Proteins, iron, phosphorus and starch) | Everyday | 104 | 69.3 | 0.206 |
| Twice a week | 36 | 24 | ||
| Once a week | 6 | 4 | ||
| Once a month | 3 | 2 | ||
| Never/can't remember | 1 | 0.7 |
Figure 5 denotes that 99 (66%) visited antenatal clinic 4-6 times, while 31 (20.7%) only managed to have 1-3 visits and 19 (12.7%) visited the antenatal clinic 7 times or more.
However, the number of antenatal visits had no significant association with birth weight (P-value was 0.278).
Figure 6 shows mothers’ folic acid and iron supplement intake during pregnancy, the majority of them (38.0%) took during both the second and third trimester [18]. Only 16.7% had intake during the first trimester only and 2.7% did not take it at all. The supplement intake was not associated with birth weight (P-value was 0.664).
Assessment of gestational illnesses
From the Table 6 below, all variables did not have a significant association with birth weight except for pre-pregnancy BMI (pvalue= 0.028). Almost half (46.5%) of the mothers had normal BMI (25.0 kg/m2-29.9kg/m2) and 0.7% had BMI above 39.9kg/m2. The majority 84% did not experience passive smoking.
Only 0.7% had a preexisting condition of diabetes mellitus and almost all (99.3%) did not have gestational diabetes mellitus. A large proportion (90%) had no hypertension at all and only 8.7% had maternal hypertension. Those that had malaria in pregnancy and were treated were 15.3%and 93.3% never experienced sexually transmitted infections.
| Variable | Indicator | Frequency | Percent | P-value |
|---|---|---|---|---|
| Cigarette smoker at home (passive smoking) | Yes | 24 | 16 | 0.960 |
| No | 126 | 84 | ||
| Hypertension | Chronic hypertension | 2 | 1.3 | 0.936 |
| YES maternal hypertension | 13 | 8.7 | ||
| NO hypertension at all | 135 | 90 | ||
| Diabetes (DM) | Chronic DM | 1 | 0.7 | 0.297 |
| NO gestational DM | 149 | 99.3 | ||
| Haemoglobinopathy (sickle cell or thalassemia) | Yes | 4 | 2.7 | 0.859 |
| No | 146 | 97.3 | ||
| Anaemia in pregnancy | Yes | 15 | 10 | 0.189 |
| No | 135 | 90 | ||
| Malaria during pregnancy | No | 127 | 84.7 | 0.758 |
| Yes, and was treated | 23 | 15.3 | ||
| STIs e.g Syphilis | Had and was treated | 4 | 2.7 | 0.857 |
| Never had | 140 | 93.3 | ||
| Had during pregnancy, treated | 6 | 4 | ||
| Pre-pregnancy BMI | 18.5-24.9 | 43 | 28.7 | 0.028 |
| 25.0-29.9 | 70 | 46.5 | ||
| 30.0-34.9 | 28 | 18.7 | ||
| 35.0-39.9 | 8 | 5.4 | ||
| >39.9 | 1 | 0.7 | ||
| Any related accident | Yes | 16 | 10.7 | 0.373 |
| No | 134 | 89.3 |
Maternal age at birth association with birth weight
Table 7 shows that there was a significant association (Pvalue= 0.035 which is <0.05) between birth weight and maternal age because 27.30% and 5.80% of mothers aged from 15-19 and 20-24 respectively had babies born under low birth weight [19]. Only 2.70% of those aged from 30-34 had low birth weight babies with none of those aged from 35-45. This showed an increase in birth weight with an increase in maternal age.
| Variable | Baby birth weight | Chi-square test asymptotic significance (P-value) | |||
|---|---|---|---|---|---|
| Indicator | Low birth weight | Normal | Macrosomia | ||
| Maternal age at birth | 15-19 | 3 | 6 | 2 | 0.035 |
| 27.30% | 54.50% | 18.20% | |||
| 20-24 | 3 | 38 | 11 | ||
| 5.80% | 73.10% | 21.20% | |||
| 25-29 | 0 | 2 | 0 | ||
| 0.00% | 100.00% | 0.00% | |||
| 30-34 | 2 | 45 | 27 | ||
| 2.70% | 60.80% | 36.50% | |||
| 35-45 | 0 | 7 | 4 | ||
| 0.00% | 63.60% | 36.40% | |||
Education level association with birth weight
It was shown that birth weight and educational level are associated. From Table 8 below, it was indicated that the majority of those who did secondary school learning and tertiary level of education had babies with normal birth weights. It was observed that 69.60% of those who reached secondary education had normal weight babies and 53.80% of those who reached tertiary education also had normal babies.
| Variable | Birth weight | Chi-square test asymptotic significance (P-value) | |||
|---|---|---|---|---|---|
| Indicator | Low birth weight | Normal | Macrosomia | ||
| Education level | Primary | 0 | 6 | 6 | 0.046 |
| 0.00% | 50.00% | 50.00% | |||
| Secondary | 8 | 78 | 26 | ||
| 7.10% | 69.60% | 23.20% | |||
| Tertiary | 0 | 14 | 12 | ||
| 0.00% | 53.80% | 46.20% | |||
BMI (pre-pregnancy) association with birth weight
The association shows that 72.10% of those with normal BMI (between 18.5 and 24.9) had babies with normal weight. However, the percentage of normal babies born from overweight (BMI 25.0 kg/m2-29.9 kg/m2) and obese (BMI 30.0 kg/m2 or more) mothers was quite reduced (around 60%) as compared to those of normal BMI (Table 9).
| Variable | Birth weight | Chi-square test asymptotic significance (P-value) | |||
|---|---|---|---|---|---|
| Indicator | Low birth weight | Normal | Macrosomia | ||
| BMI (Kg/m2) | 18.5-24.9 | 3 | 31 | 9 | 0.028 |
| 7.00% | 72.10% | 20.90% | |||
| 25.0-29.9 | 4 | 44 | 22 | ||
| 5.71% | 62.86% | 31.43% | |||
| 30.0-34.9 | 0 | 18 | 10 | ||
| 0.00% | 64.30% | 35.70% | |||
| 35.0-39.9 | 0 | 5 | 3 | ||
| 0.00% | 62.50% | 37.50% | |||
| 40 and above | 1 | 0 | 0 | ||
| 100.00% | 0.00% | 0.00% | |||
Gestational period association with birth weight
From the babies born between 37 and 39 weeks gestation, 15.4% had low birth weight while those with a gestational age of 40 weeks and more had only 3.20% of low birth weight (Table 10).
| Variable | Birth weight | Chi-square test asymptotic significance (P-value) | |||
|---|---|---|---|---|---|
| Indicator | Low birth weight | Normal | Macrosomia | ||
| Gestational age at birth | 37 weeks-39 weeks | 4 | 19 | 3 | 0.008 |
| 15.40% | 73.10% | 11.50% | |||
| 40 weeks and beyond | 4 | 79 | 41 | ||
| 3.20% | 63.70% | 33.10% | |||
The prevalence of low birth weight was relatively low compared with previous studies. More than half of the babies were normal weight (more than 2500 g as stipulated by the World Health Organization). The demographic health surveys data in Zambia showed that from the year 2013 to 2014 about 9% of neonates were born with low birth weight. Further studies in 2017 showed that nearly 11% of neonates in the largest health system in Zambia-Lusaka met WHO criteria for LBW.
Therefore the prevalence of low birth weight as found in this study had decreased in comparison with previous studies. This reduction can be attributed to the fact that low birth weight has been a major determinant of infant mortality and morbidity public in developing countries for several years and since then, identification and prevention of the risk factors including maternal factors are being put in place [20].
Maternal nutrition over the years has been identified as one of the main determinants of low birth weight. In this study, however, none of the maternal nutritional factors was significantly associated with birth weight. The reason for this is that almost all mothers understood the importance of good and healthy nutrition during pregnancy and as a result, a relatively large percentage of mothers consumed a range of the foods daily compared to those who consumed once less frequently. The measurement of nutrients in this study was by reported data from answered questions on the type and frequency of foods eaten during pregnancy. This measurement was based on reported data and therefore not objective. The factors such as the foods being overcooked or undercooked were not accounted for. This might also explain the statistical insignificance relation with birth weight because nutritional intake during pregnancy, has the potential to influence birth outcomes including birth weight.
The findings of this study contrast another study that was done to investigate the effect of maternal nutritional status on birth weight. The study showed that maternal nutritional status impacted significantly on newborn birth weight as poorly nourished mothers were observed to produce a higher percentage of LBW babies when compared to those who were better nourished. However, the factors used to determine maternal nutritional status were weight gain in pregnancy, haemoglobin and serum albumin which are different from the ones used in this study. The only factors established to have had an association with maternal nutrition were maternal age, educational level, BMI and gestation age at delivery. Birth weight increases with an increase in maternal age as older women have much more developed physiology equipped for proper fetal development than the younger ones. This study found the same correlation. Teenage mothers had a higher percentage of low birth weight babies compared with non-teenage mothers. The much older mothers did not have any low birth weight babies.
Those who attained secondary school level and tertiary education had a much higher percentage of normal birth weight babies compared with those that only had primary level school education. More knowledgeable women are likely to have an in-depth understanding of the maternal factors and requirements for proper fetal growth, development and outcome as observed in resource poor settings. It was therefore deduced that the lower the education level attained, the lower the prevalence of normal weight babies. Since most studies have shown the effect of maternal BMI and weight gain in pregnancy on birth weight, this study explored BMI before pregnancy to examine its role on birth weight. It was found that a larger percentage of mothers with normal pre-pregnancy BMI had normal birth weight babies compared to those that had overweight and obese. A normal value of pre-pregnancy BMI corresponded with reduced low birth prevalence. This serves to notify the importance of maintaining good nutrition even before pregnancy as the maternal nutritional status will greatly depend on the pre-pregnancy nutritional status.
According to the World Health Organization, a preterm baby is a baby born alive before 37 weeks of gestation. Preterm babies were not considered in this study as they would most with no doubt be born with low birth weight. The babies who were born at 40 weeks gestation and beyond had a lower prevalence of low birth weight compared to those that were born between 37 weeks and 39 weeks gestation. Therefore, the lesser the gestational age at birth the higher the prevalence of low birth weight.
The prevalence of low birth weight being 5.3% indicated a decrease over the past years which showed that some interventions are certainly being put in place to overcome this public health problem. In as much as no association was established between the maternal diet and nutritional factors with birth weight, many studies over the years have shown that there is a significant relationship between maternal nutritional status and low birth weight. Factors such as maternal age, education school level, BMI and gestational age at delivery however had an established relationship with low birth weight in correlation with other findings from other studies on maternal factors of birth weight. Low birth weight prevalence decreases with an increase in maternal age while the lower the educational level attained, the lower the prevalence of birth weight. A normal value of pre-pregnancy is associated with a reduced prevalence of low birth weight and an increase in gestational period reduces the prevalence of low birth weight. Therefore, the challenge of addressing the problem of low birth weight remains an urgent imperative for development as it is a major determinant of infant morbidity and mortality in developing countries.
Based on the findings of this study, the following are the recommendations offered as a step to solving the public health problem of low birth weight in Zambia:
• Promote activities in the community that provide sexual and reproductive health information to sensitize on the dangers of adolescent pregnancies.
• Promote clinic based women’s nutrition groups as sources of information for healthy diets with emphasis placed on the importance of maintaining a normal BMI even before pregnancy.
• Promote programs and NGOs that seek to empower school education among young women by providing out-of-school girls with education opportunities.
• Provide early screening facilities that help with the early detection of signs of early birth to provide the necessary interventions to prevent it.
First and foremost, I would like to acknowledge the almighty god for giving me unending wisdom, strength and good health during my project proposal development period. It was not out of my own capabilities but through his inspiration of academic excellence. My great thanks and acknowledgement goes to the public health unit lecturers particularly Professor Seter Siziya and Mr. Nyirenda Tato for their attention and time given to me during the consultation period for this proposal. Special thanks go to my supervisor Dr. David Mulenga for the supervision and guidance given to me and to my best friend Mwamba Kapambwe who created a fresh and unstressful academic atmosphere for me. Their efforts to this piece of work will always be appreciated.
The author sought ethics clearance and approval from the Tropical Disease Research Centre (TDRC) ethics committee at Ndola teaching hospital. To conduct the study, legal permission was sought from the national health research authority, copperbelt provincial health office and Ndola district health office. There were no immediate study benefits to the participants. However, many people may benefit in future if the recommendations of this study are implemented using the correct measures to reduce low birth weight and consequently neonatal morbidity and mortality. There were no risks associated with participating in this study as the procedure only involved obtaining information from the participants using the questionnaires.
The respondents were assured of confidentiality and respect by stating out that the information gathered from the study would strictly adhere to regulations in the participant information sheet and would have no names attached to it.
No one was forced to take part in the study and individuals were at liberty to either participate or not or to withdraw from the interviews at any point, for whatever reason they might have had. Informed consent was obtained from the respondents by reading and explaining to them the relevant information as stipulated on the participant information sheet. All questions from the participants were answered to ensure their full comprehension and written consent was eventually obtained by signing.
There were not many limitations in this study. However, there was some recall bias especially when it came to remembering the types of foods consumed in the early stages of pregnancy. To counteract this limitation, mothers were allowed enough time to think through their responses. Critical measurements such as birth weight and maternal height were taken care of through the use of recorded information on the postnatal card as it contained even information during pregnancy. However, the weight of the mother before pregnancy was based on reported responses which also had some recall bias. This was also dealt with by patiently taking the respondents through back to the time when they were not pregnant.
I, Kisa Martha Nakana, hereby do declare that this study is my own piece of work and that it has not been partially or wholly presented before for any degree or examination in any university or college. All the sources of information used or quoted have been thoroughly cited and acknowledged as complete references. Dr. David Mulenga hereby declares that I have checked this project proposal and that it is the original work of the author. I, therefore, approve that it should be submitted for assessment.
This piece of work is highly dedicated to my family especially my father Andrew Sikana, mother Edinah Sikana, young brother Tenson Sikana and not forgetting my very best friend Mwamba Kapambwe. These people are and have been a great blessing and encouragement to my life. Their tireless effort towards my life and wellbeing has contributed greatly to me reaching this level. May the good lord continue to bless them.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Journal of Clinical Research received 11 citations as per Google Scholar report