Research Article - (2023) Volume 8, Issue 1
Received: 14-Dec-2022, Manuscript No. PE-22-83547;
Editor assigned: 16-Dec-2022, Pre QC No. P-83547;
Reviewed: 29-Dec-2022, QC No. Q-83547;
Revised: 04-Jan-2023, Manuscript No. R-83547;
Published:
12-Jan-2023
, DOI: 10.37421/2157-1042.2022.8.161
Citation: Krumpl, Günther and Evelyn Walter. “Cost-effectiveness of landiolol, an Ultra-short-acting Beta-blocker, for Treatment of Sepsis Related
Tachyarrhythmia in Germany.” Pharmacoeconomics 8 (2023): 161.
Copyright: © 2023 Krumpl G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Sources of funding : This study was funded by a grant from Amomed Pharma GmbH, Austria.
Background: Sepsis and septic-shock are associated with cardiovascular problems, including tachyarrhythmia, myocardial injury, and changes in vascular endothelial function that might affect cardiac output with potential fatal outcome. The consequences of sepsis extend well beyond the acute illness. Tachycardia and new-onset atrial-fibrillation (AF), often treated with less effective agents such as amiodarone, are key prognostic factors for sepsis and associated with increased use of health-care resources and costs. Early decrease of heart-rate is associated with improved outcome. The use of β-blockers for managing acute arrhythmias in patients with septic-shock has been described in the literature. Landiolol, an ultra-short-acting β1-selective adrenergic-receptor-antagonist, is used specifically for the acute management of atrial-fibrillation and atrial-flutter in critically ill patients with/without cardiac-dysfunction.
Methods: A decision-model was developed to reflect the cost-effectiveness of landiolol in addition to conventional-therapy vs. standard-of-care (SoC) to manage sepsis-related tachyarrhythmia. The model combines a short-term decision tree to describe the time span of the sepsis related hospitalization over 28 days. The endpoint of the decision tree was then combined with a Markov model to simulate a life-long time horizon, as AF and post discharge mortality occurrence following sepsis hospitalization was more common among patients with new-onset AF during sepsis. The model calculates total costs (incl. hospital-stay, ICU and ventilation, AF costs) quality-adjusted life-years/QALYs and life-years/LYs over life-time.
Results: Manage sepsis related tachyarrhythmia with landiolol led to estimated lifetime costs of 59.130.79 € (95%-CI=53,436-64,901) per patient and 4.02 QALYs (5.56 LYs) over a life-time horizon. SOC was associated with 60.935.11 € (95%-CI=47,928-73,124) and 3.55 QALYs (5.01 LYs). Landiolol yields cost savings of about 1,804.31 € per patient and a QALY gain of 0.47 or 5.63 months in perfect health. Landiolol resulted in a life year gain of 0.54 LYs.
Conclusion: The economic analysis shows that the use of landiolol is associated with costs saving from the payer’s perspective.
Sepsis • Atrial fibrillation • Landiolol hydrochloride • Cost effectiveness
Sepsis is the extreme form of a body reaction to an infection leading to a life-threatening condition which most often triggers in patient treatment and thus high medical costs which increase with the severity of the disease [1].
Severe inflammation, being the reason, and within short time, the consequence of the release of cytokines and diverse other mediators, triggers severe vascular leakage and cardial dysfunction eventually leading to hypotension, tachycardia and finally myocardial depression and cardiovascular shock [2,3].
Due to a multifactorial upregulation of the sympathetic nerve system, the plasma levels of endogenous catecholamines are elevated in patients with sepsis [4] which, when prolonged and excessive, can induce substantial adverse effects [5]. In some patients, volume substitution and the sympathetic reflex reactions may not adequately correct the detrimental cardiovascular reaction and, due to persistent hypotension, external vasopressors have to be administered [6]. According to the Surviving Sepsis Campaign, norepinephrine should be used as first line vasopressor and arginine-vasopressin as the second line [7].
In an intensive care unit (ICU) sepsis is a frequent diagnosis [8]. Sepsis incidence varies within the western countries between 7% and over 30% whereby in the past years, the incidence increased, the mortality decreased but due to the higher frequency, the overall sepsis-death rate rose [9]. In sepsispatients mortality is related to many factors such as vasopressor demand [10], lactate level [11] and excessive elevation of heart rate in relation to the body temperature [12]. Arrhythmias, specifically new onset AF (NOAF) are both a marker of disease severity as well as a likely contributor to poor outcomes [13], for instance by inducing stroke [14].
The cumulative risk of NOAF was 10%, 22% and 40% in patients with sepsis, severe sepsis and septic shock, respectively [15]. NOAF increases the length of stay and cost burden of ICU-patients [16] and mortality after discharge [17].
Beta blockers are frequently used for treatment of tachycardia and AF and have been shown to be superior to calcium channel blocker, digoxin, and amiodarone in reduction of in hospital mortality in septic patients [18]. A meta-analysis of 14 prospective or controlled trials showed similar results across studies regarding the beneficial effects of beta-blockers on tachycardia in patients with sepsis, without clinically or statistically significant effects on blood pressure [19].
Landiolol, a ultra-short acting ß1-selective antagonist, has proven to be effective against tachyarrhythmias [20]. In the EU it is approved for treatment of supraventricular tachycardia and for the rapid control of ventricular rate in patients with atrial fibrillation or atrial flutter in perioperative, postoperative, or other circumstances where short-term control of the ventricular rate with a short acting agent is desirable [21]. With a ß1/ß2-receptor activity ratio of greater than 200 and an onset of action between 1-6 minutes and an offset of action between 5-10 minutes after end of infusion, landiolol is a highly adjustable and easily titratable ß-blocker [20-23]. Landiolol neither blocks Na, Ca and K channels nor decreases plasma renin levels and thus exerts less effect on left ventricular function and blood pressure [24]. In addition, landiolol has no pharmaco-chaperoning activity and thus less potential for drug tolerance and rebound tachycardia after infusion stop [22,23].
In a historical cohort study landiolol has been used successfully in septic patients with supraventricular tachyarrhythmias. Compared to conventional treatment (Amiodarone, diltiazem, other beta blocker, disopyramide) landiolol decreased the heart rate significantly faster and converted significantly more patients into sinus rhythm without alterations of the blood pressure [25].
Recently landiolol was also used in prospective multicenter, open label randomized trial (J-Land 3S) compared to conventional therapy in 151 patients with sepsis and tachyarrhythmia [26]. A significantly larger proportion of patients in the landiolol group had a heart rate of 60–94 bpm 24 h after randomization (primary endpoint) than in the control group (55% [41 of 75] vs. 33% [25 of 75]), with a between-group difference of 23.1% (95% CI 7.1–37.5; p=0.0031). New onset arrhythmia over 168 h after randomization showed a significantly lower incidence in the landiolol group [9% (7 of 75) vs. 25% (19 of 75); p=0.015, with a hazard ratio (HR) of 0.357 (95% CI 0.150–0.849)]. 28-day mortality was lower in the landiolol group [(12% [9 of 75] vs. 20% [15 of 75]; p=0.22, HR of 0.599 (0.262–1.370), not significant]. Adverse events [64%] vs. [59%] and serious adverse events [12%] vs. [11%] were similar between the landiolol group and the control group, respectively. The main adverse event in the landiolol group was hypotension [12%] which was easily controlled by dose reduction or termination of infusion.
In the light of the substantial financial costs induced by the treatment of sepsis and septic shock, we undertook to analyze the cost-effectiveness of landiolol vs. standard of care (SoC) for treatment of sepsis related tachyarrhythmias in tensive care patients with sepsis or septic shock using the data of the above-mentioned trial [26]. In addition, we also undertook to investigate the health economic aspects of the long-term outcome, since post discharge mortality is elevated following sepsis hospitalization in patients with new-onset AF during sepsis [17].
Decision analytical techniques were used used to estimate the costeffectiveness of landiolol vs. SOC, which is a well-accepted methodology and has been used in several published studies calculating the costs of medical strategies. The model combines a short-term decision tree to describe the time span of the sepsis related hospitalization over 28 days. The endpoint of the decision tree was then combined with a Markov model to simulate a life-long time horizon. The model was developed using Microsoft Excel and it calculates and compares the costs and outcomes for a virtual cohort of patients.
Decision analytical techniques combine data from many sources (RCTs, epidemiologic data, costing data and expert opinion, etc.) to produce detailed estimates of the clinical and economic consequences of different therapeutic alternatives, thus permitting to represent the complexity of the real world in a simpler and comprehensive form and simplifying and evaluating complex decision problems as an aid in the decision-making process [27].
A decision tree consists of a series of branches, each representing different options (decisions or events) that arise at different points, referred to as nodes (e.g., decision nodes and chance nodes). In effect, a model shows the consequences and complications of different therapeutic interventions, and it should correspond as much as possible to the real-life situation of the disease in each setting.
The decision tree was developed based on a single clinical trial, the J-Land 3S trial of Kakihana Y, et al. [26]. The J-Land 3S trial is a multicenter, openlabel, randomized controlled trial at 54 hospitals in Japan. Patients admitted to the intensive care units (ICU) who received conventional treatment for sepsis, according to clinical guidelines for the management, and who subsequently developed a tachyarrhythmia, were enrolled. The primary outcome was the proportion of patients with heart rate of 60–94 bpm 24 h after randomization. Patients without heart rate data 24 h after randomization were handled as non-responders. Secondary efficacy outcomes included changes in heart rate, proportion of patients with a decrease in heart rate of 20% or more (baseline and 24 h, 48 h, 72 h, and 96 h after randomization), proportion of patients whose heart rate was controlled to 60–94 bpm (up to 96 h), proportion of participants with new-onset arrhythmia (by 168 h), ICU free days (by 28 days), hospital-free days (by 28 days), 28-day mortality, and clinically relevant parameters [26].
Patients with sepsis or septic shock enter the model and receive either landiolol or SoC (decision notes). Patients either reach the heart rate target of 60–94 bpm within 24 hours or they do not reach it; patients may experience an arrythmia or not (chance node) and could subsequently die (end node) (Figure 1).
Figure 1. Decision tree. The square is a decision node from which the competing strategies originate. The circles are chance nodes from which a study result leads to a particular management of the patient. The triangles are the endpoints of each pathway and represent the final outcome (additional costs per death case saved (a), additional costs per new-onset of arrhythmia cases avoided (3) and costs per patient reaching heart rate target (c)) of the particular pathway.
To estimate the long-term consequences, a Markov model consisting of 3 health states was developed: (1) No arrythmia (no AF), (2) AF or (3) death (Figure 2) was developed. According to specific transition probabilities defined as yearly incidences, patients may move from the health state No AF to the AF state and suffer from a new-onset arrhythmia or remain unchanged. From each health state a patient has a probability to die. If a patient dies, he will move to the dead state and remain there for the rest of the simulation (Table S1).
The progression from t = n to t = n + 1 is called a cycle. All clinically important events were modelled as transitions from one state to another. Probabilities were associated with each change between two states; these were termed transition probabilities. Each transition probability was a function of the health state and the treatment. Patients were followed through the model over 33 year (mean age of 67 years plus 33 years).
The aim of the model was to evaluate the benefit of landiolol to reduce mortality and avoid new-onset arrhythmia in patients experiencing sepsis related tachyarrhythmia. Patients with sepsis related tachyarrhythmia experienced a higher incidence of mortality, morbidity, a longer hospital length of stay (LOS) including ICU and more frequent readmissions and finally higher costs.
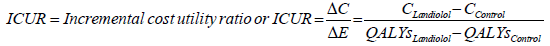
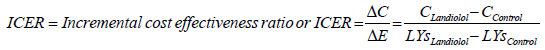
Resource use (RU) was derived from the clinical trial, the literature and German hospital data. Costs were calculated from the payer’s perspective for the year 2020. The model outcomes present cumulative costs, clinical outcomes expressed as quality adjusted life years (QALYs) saved, life-years saved, AF avoided. The incremental cost-effectiveness ratio (ICER) can be interpreted as additional costs or savings per QALY gained. Probabilities and utilities were derived from the literature. QALYs, LYs and total costs were discounted at 3% per year. The model was developed over a life-time horizon. To assess the robustness of our findings, we carried out deterministic and probabilistic sensitivity analyses. The analysis was conducted in consideration of the Modeling Good Research Practices published by the ISPOR Task Force [28].
Target population
Both groups were similar in terms of patient age, baseline arrhythmia, hemodynamic parameters, and presence of septic shock, APACHE II, and SOFA score. 90 (60%) of 151 patients were male and 61 (40%) were female, with a mean age of 67.1 years (SD 14.5).The mean heart rate at randomization was 117.5 bpm (SD 14.0). Baseline tachyarrhythmia was sinus tachycardia in 121 (80%) of 151 patients and AF in 29 (19%). Most patients had septic shock (137 [91%] of 151), mean APACHE II score was 22.7 (SD 278.7), and mean SOFA score was 10.1 (SD 3.0). The most common sites of infection were the respiratory system (45 [30%]), abdomen (34 [23%]) and urinary tract (24 [16%]) [26].
Decision tree
The clinical data of the decision tree primary focuses on the clinical outcomes from the J-Land 3S study (Table 1).
| Decision Tree (short term) | Landiolol | Control | Source | ||
|---|---|---|---|---|---|
| Patients with heart rate of 60–94 bpm at 24 h | 54.7% | 33.3% | Kakihana Y, et al. [26] | ||
| Patients with new-onset arrhythmia by 168 h | 9.3% | 25.3% | |||
| Patients with new-onset of AF | 5.3% | 14.7% | |||
| Prior AF | 19.0% | 19.0% | |||
| Deaths per day 28 | 12.0% | 20.0% | |||
| Markov Model (long term) | Landiolol | Control | Source | ||
| Re-hospitalisation 365 days | 39% | 39% | Shankar‑Hari M, et al. [31] | ||
| Postdischarge Identification of AF by AF | No AF | New-on-set AF | Prior AF | Walkey AJ,et al. [17] Transition probability were derived on the basis of these data (Table S1) |
|
| Status During Sepsis | |||||
| 1st year | 7.7% | 44.2% | 57.2% | ||
| 2nd year | 10.5% | 49.3% | 60.9% | ||
| 3rd year | 12.6% | 52.0% | 62.3% | ||
| 4th year | 14.3% | 53.6% | 63.1% | ||
| 5th year and + | 15.5% | 54.9% | 63.1% | ||
| Mortality Following Discharge from Sep-sis Hospitalization | |||||
| HR* | HR** | HR** | Wang HE, et al. [29] Walkey AJ,et al. [17] |
||
| 1st year | 13.07 | 1.04 | 1.19 | ||
| 2nd year | 2.64 | 1.04 | 1.19 | ||
| 3rd year | 2.18 | 1.04 | 1.19 | ||
| 4th year | 1,97 | 1.04 | 1.19 | ||
| 5th year and + | 2.08 | 1.04 | 1.19 | ||
| 1.41 | 1.04 | 1.19 | |||
New-onset arrhythmia
The first change node of the decision tree distinguishes between patients who suffer a “New-onset arrhythmia” and who did not. The secondary efficacy outcomes included proportion of participants with new-onset arrhythmia (by 168 h). Landiolol was associated with a lower incidence of new-onset arrhythmia after randomization, namely 9,3% [7 of 75] vs. 25,3% [19 of 75]; p=0·015, with a hazard ratio [HR] of 0.357 (95% CI 0.150–0.849). The most frequent type of arrhythmia was AF (5% [4 of 75] vs. 15% [11 of 75] [26].
Mortality rate
The J-Land 3S study has documented 28-day mortality. Mortality did not significantly differ between groups. 12% (9 of 75) of patients in the landiolol group died within the observation period, compared to 20% (15 of 75; p=0·22) in the control group. The HR amounts to 0.599 (95% CI 0.262–1.370) [26].
Markov-Model
The clinical data of the long-term follow-up were modelled based on data published by Walkey AJ, et al. [17]. The authors had analyzed the long-term outcome of a Medicare sample of 138,722 sepsis survivors associated newonset AF. The study determines 5-year risks of AF occurrence, heart failure, ischemic stroke, and mortality after the sepsis hospitalization, according to AF status during the sepsis admission. We use the 5-year data of AF occurrence and mortality for our model. All clinical data were displayed in (Table 1).
Post discharge identification of AF
According to the data set, AF occurrence following sepsis hospitalization was more common among patients with new-onset AF during sepsis (54.9%) than in patients with no AF during sepsis (15.5%) over a 5-year time horizon. Based on the presented data transition probabilities were conducted for the year one to year five. After five years constant transition probabilities were assumed. Over time, the probability of developing an AF decreases [17].
Post discharge mortality
When compared with patients without AF, patients with new-onset AF during sepsis had a greater risk of post-sepsis hospitalization mortality (5-year unadjusted risk, 74.8% vs. 72.1%: multivariable adjusted hazard ratio (HR), 1.04 (95% CI, 1.01-1.07). In case of patients with prior AF the adjusted HR amounts to 1.19 95% (95% CI, 1.17-1.21). The long-term mortality following a sepsis was analyzed by Wang HE, et al. [29]. Based on a multivariable analysis, the association of sepsis with increased all-cause mortality persisted for up to 5 years, after adjustment for confounders. HR were published which compare the mortality after sepsis with the overall population. These HR were used for patients without AF.
Resource use and cost assessment
The cost assessment is based on the assignment of costs to the health states. The costs of each health state are determined by the resource utilization associated with a health state. Resource use (e.g. the type and frequency of medical goods and services rendered to the patient) and monetary value (prices, tariffs and/or opportunity costs) for each unit of medical goods and services were used to calculate the total direct costs. In order to estimate the cost of managing sepsis related tachyarrhythmia in Germany, only direct costs were included in the analysis. Direct medical costs were collected from a payer’s perspective.
The analysis collects hospital stay costs, ICU stay costs and ventilation costs during ICU stay due to sepsis related tachyarrhythmia. Medication costs for managing sepsis related tachyarrhythmia are covered in the German G-DGR lump sum. Finally, AF costs of the long-term follow-up were integrated. All costs were derived from public price lists, tariff catalogues and the literature. Follow-up costs were discounted with a 3% discount rate.
The hospital length of stay (LOS) was derived from the J-Land 3S trial data. The clinical trial has calculated the number of hospital free days during the 28 days after randomization by treatment arm. The number of hospital-free days was similar in both groups. 1.6 hospital-free days were documented for patients receiving landiolol and 1.8 days for SOC patients (p= 0·91) (26). LOS data for the hospital length of stay was displayed in (Table 2).
| Decision Tree (short term) | Landiolol | Control | Source |
|---|---|---|---|
| Hospital days | 26.4 | 26.2 | Kakihana Y, et al. [26] |
| ICU days | 13.4 | 14.7 | |
| Days with ventilation | 11.0 | 10.1 | |
| Hospital stay of sepsis, septic shock (costs per day) | 613.47 € | G-DRG 2020 see table S2 | |
| ICU costs without ventilation | 1,392.43 € | Martin J,et al. [30], inflated | |
| ICU costs with ventilation | 1,734.15 € | Martin J,et al. [30], inflated | |
| Markov Model (long term) | Costs | Source | |
| Costs of AF per year | 3,781.54 | Reinhold T, et al. [32] | |
| Utilities | Utility value per year | Source | |
| Adults in the ICU | 0.53 | Westwood M, et al. [34] | |
| Adults hospitalized | 0.68 | Westwood M, et al. [34] | |
| Septic shock survivor | 0.75 | Lam SW, et al. [35] | |
| Disutility AF | -0.08 | Chang AY, et al. [36] | |
Costs of hospital stay were derived from the G-DGR catalogue. All relevant G-DGR codes were selected to calculate an average value for cost per hospital stay. Points per G-DRG code were multiplied with the 2020 baserate of 3,679.62 Euro per point.
For the duration of ICU stays the same recording approach was applied. The number of non-ICU days during the 28 days after randomization was calculated by treatment arm. The number of ICU-free days was similar in both groups. In the landiolol group patients exhibit 14.6 ICU-free days, compared to 13.3 days in the control group (p=0.55) [26].
An overview of ICU days is shown in (Table 2).
The number of ventilator free days during the 28 days after randomization was recorded for both treatment arms. 17 ventilation-free days were documented for patients receiving landiolol and 17.9 days for SOC patients (p= 0·47) [26] (Table 2).
Days with ventilation for the comparator groups were displayed in Table 2.
Costs for an ICU day were retrieved from the literature.
Martin J, et al. [30] have published costs per day and distinguish between patients require mechanical ventilation and patients without ventilation. The aim of this study was to determine resent costs per intensive day in Germany using cost calculation, which was carried out based on the routine data of the data management system (PDMS) of a hospital. Cost assessment concluded that cost per day with mechanical ventilation amounts to 1,426 € per day and is 281 € higher than for days without mechanical ventilation (1,145 €). Inflated costs per ICU day, amounts to 1,388,48 € and with mechanical ventilation 1,729,33 €. The calculation takes into consideration that 39% of sepsis survivor are re-hospitalized within 365 days [31].
Patients in both groups received conventional therapy, including respiratory and fluid resuscitation, antimicrobials, and catecholamines, that were deemed necessary by the attending physician, with the exception of prohibited drugs. beta-blockers, class IV antiarrhythmic and digitalis were prohibited through to 96 h after the onset of tachyarrhythmia, except for treatment of adverse events or if judged by the investigator to be necessary [26].
Patients in the landiolol group also received landiolol using the following dosing schedule: The administration of landiolol was mandatory for the first 96 h after randomization and optional between 96 h and 168 h after randomization. Landiolol hydrochloride was infused intravenously at an initial dose of 1 μg/ kg per min within 2 h after randomization. The dose of landiolol was to be increased by 1 μg/kg per min generally every 15–20 min, until the heart rate decreased to less than 95 bpm. From 96 h to 168 h after randomization (optional administration), the dose of landiolol was adjusted in increments or decrements of 1 μg/kg per min. The maximum permitted dose was 20 μg/ kg per min, which was based on findings of previous studies. After 96 h, the patient could be transitioned to orally or percutaneously administer betablockers. The dose of landiolol was to be reduced or discontinued in patients with a decrease in systolic blood pressure of 20% or more from randomization or heart rate of less than 60 bpm [26].
The used concomitant medications were displayed in Table S3.
Medication costs are included in the diagnosis-related group (DRG) costs and represent not a single cost component.
AF costs used for the calculations of the long-term follow-up were derived from the literature. Reinhold T, et al. [32]. Have published a study with the aim to describe the resource consumption associated with AF and to measure costs of direct treatment as well as consequential costs in Germany. The analysis is based on the representative ATRIUM register (Ambulantes Register zur Morbidität des Vorhofflimmerns, Ambulatory register on morbidity of atrial fibrillation) a prospective, multicenter cohort study in which general practitioners and family doctors documented the characteristics and resource utilization of consecutively enrolled patients. Results revealed inflated 2020 disease-specific mean costs of 3,781.54 Euro.
Health state utilities
Utilities are a measure of preference between health states where preference can be equated with value or desirability. Utilities for health states included in the model were obtained from international literature, and, if necessary, re-expressed on a utility scale from 0 to 1 (where 0 represents death and 1 represents full health) by using weighting factors. The QALY (Quality-adjusted life years) concept allows combining the effects of health interventions on quantity and quality of the remaining life years into a single index. QALYs are calculated by multiplying the length of time spent in a certain health state by the utility score associated with it [33].
Utilities for a sepsis related hospitalisation were derived from an NHS Health technology assessment [34]. The utility for sepsis survivor was retrieved from a recent health economic evaluation [35] as was the data for the disutility of AF [36]. All utilities are presented in Table 2.
Sensitivity analysis
A deterministic one-way sensitivity analysis (OWSA) was performed to assess how variations of individual input parameter values affect the model output, specifically, the resulting incremental cost-utility (ICUR). This analysis was used to judge the robustness of our findings. Input ranges for sensitivity analysis were obtained from 95% CI or adding/subtracting percentage values to or from the baseline estimates (±20% for costs and ±10% for clinical input data).
In addition, a probabilistic sensitivity analysis was performed, which allows the contribution of each parameter to model outcomes to be investigated, while also considering the uncertainty of other model parameters. For this purpose, we incorporated a probability distribution of the input variables. A second order Monte Carlo simulation was performed for 500 hypothetical patients based on the distributions of all input variables; gamma distribution for costs and beta distribution for probabilities and utilities.
Patients with sepsis-related tachyarrhythmia had a higher incidence of mortality, morbidity and LOS including ICU, a more frequent ventilation requirement and finally higher costs. Total costs include hospitalization costs plus ICU, and ventilation costs. Manage sepsis related tachyarrhythmia with landiolol led to estimated lifetime costs of 58,100.71 € (95%-CI=52,902- 63,670) per patient and 4.02 QALYs (5.56 LYs) over a life-time horizon. SOC was associated with 60.935.11 € (47,928-73,124) and 3.55 QALYs (5.01 LYs). Landiolol yields cost savings of about 2,834.40 € per patient and a QALY gain of 0.47 or 5.63 months in perfect health. Landiolol resulted in a life year gain of 0.54 LYs. An in-depth analysis shows that the major proportion of cost reduction is associated with reduced need of ICU care (-1,502.60 or -1.3 days). Those who received landiolol also exhibit cost savings for not experiencing AF in the following year of 1,629.14 €. Total savings offset medication costs for landiolol of 1.156,00 €. New-onset AF occurred in 5.3% of cases in the landiolol group and new-onset arrhythmia decreased by 64%. Over live-time additional 9.3% of sepsis survivor remains AF free. The landiolol strategy, marked as “Dominant”, shows it saves money and improves outcomes compared to SOC (Table 3).
| Cost Components | Landiolol | Control |
|---|---|---|
| Costs hospital stay (normal ward) | 16,195.69 | 16,072.99 |
| Costs ICU stay | 22,417.44 | 23,920.04 |
| Re-hospitalization | 13,252.02 | 12,047.30 |
| AF costs | 6,235.55 | 8,894.78 |
| Total costs | 58,100.71 | 60,130.68 |
| QALYs | 4.021 | 3.552 |
| Difference in POAF onset | 0.47 | |
| Additional costs/savings per QALY (ICUR) | DOMINANT | |
| LYs | 5.557 | 5.014 |
| Difference in POAF onset | 0.543 | |
| Additional costs/savings per LY (ICER) | DOMINANT | |
 |
||
 |
||
Deterministic one-way sensitivity analysis
Results were expressed as incremental costs per QALYs gained. Tornado diagrams (Figure 3) where chosen to display the results. The generated incremental cost utility ratios (ICURs) of landiolol vs. SOC ranged from -4.731, 37 to -7.340, 83 €. Landiolol remains the dominant strategy in all variations of the OWSA. The variations with the highest magnitude of influence are ICU costs without ventilation, AF costs and the number of ICU days. The base case results were confirmed in the sensitivity analysis. Tornado diagrams are presented in (Figure 4).
Figure 3. Deterministic sensitivity analysis visualized as Tornado plots. Deterministic sensitivity analysis was used to identify the critical variables affecting risk analysis. Results are displayed as Tornado diagrams, where each bar represents a one-way sensitivity analysis, and width of bars represents impact on model results. The ICUR per patient is plotted on the x-axis.
Figure 4. Probabilistic Sensitivity Analysis: The Scatterplot shows results of the Monte Carlo probabilistic sensitivity analysis for 500 patients. Incremental cost is plotted on the Y-axis, incremental effectiveness is plotted on the X-axis. Location of majority of points in the lower right area shows that majority of simulations yields cost saving and improved health outcomes. Landiolol dominates SOC. The base case results attesting the model low levels of uncertainty.
Probabilistic sensitivity analysis
The incremental costs of landiolol were plotted against SOC. All points are located in the lower right area, which denotes that all simulations yield cost savings and improved health outcomes. Mean incremental QALYs gained from landiolol were 0.466. Mean incremental costs were - 2,605 €. The resulting probabilistic ICUR from 500 iterations was -5,587 €. Probabilistic results were consistent with the results from the deterministic base case. The resulting scatter plots (Figure 5) reveal that landiolol outperforms SOC in sepsis patients. It was observed that in case of a willingness-to-pay (WTP) of 25,000 €, 94.6% of the simulations show a cost-effective result; in case of a WTP of 30,000 €, 97.2% of simulations are cost-effective.
Sepsis was identified globally as a health priority. In 2017, the World Health Assembly and the World Health Organization adopted a resolution to improve the prevention, diagnosis, and management of sepsis [37]. The resolution urged the United Nation Member States to implement measures to reduce both the human and health economic burden of sepsis [38]. The valid evidenceand consensus-based interdisciplinary guideline of the classification S3 of the German Sepsis Society should be viewed as an instrument for improving and quality assurance of the prevention, diagnosis, therapy, and aftercare of sepsis. It is aimed at all professional groups concerned with it [39]. In this context and due to understand the disease burden of sepsis and the associated health economic consequences, it is necessary to extend health economic analyses from the inpatient acute care perspective by long-term follow-up, which encompasses long-term risk of death, readmissions, cardiovascular disease, cognitive impairment, and quality of life (QOL) alterations in sepsis survivors. In addition to the health-related quality of life impairments many former sepsis patients suffer from functional limitations known for more than two decades as Critical Illness Polyneuropathy (CIP) and Critical Illness Myopathy (CIM). More than 70% of patients with septic shock and more than 60% of mechanically ventilated patients and patients with severe sepsis show significant electrophysiological changes just three days after admission to ICU [39]. These aspects should also be included in health economic evaluations. There have been numerous evidence concerning cost effectiveness of different sepsis interventions including early goaldirected therapy, fluid therapy, and corticosteroids, to support decision makers in which interventions deliver value for money in the context of limited health care resources [38]. A systematic review from Higgins and colleagues [38] identified 46 economic evaluations. Incremental cost effectiveness ratios (ICERs) ranged from dominant (lower costs and higher effectiveness) to $ 39,944/QALY (2018 USD); 17 studies used a lifetime horizon and 12 evaluations reported incremental cost per QALY with ICERs [38]. The aim of this evaluation was to analyze the cost-effectiveness of landiolol vs. SoC for treatment of sepsis related tachyarrhythmias in patients with sepsis or septic shock admitted to intensive care units using the clinical data of J-Land 3S trial. This study found that landiolol, an ultra-short-acting β1-selective antagonist, resulted in significantly more patients with sepsisrelated tachyarrhythmia achieving a heart rate of 60–94 bpm at 24 h. This was accompanied by a lower incidence of new-onset arrhythmia [26]. In addition, the health economic evaluation should include the long-term outcomes, as AF and post discharge mortality occurrence following sepsis hospitalization was more common among patients with new-onset AF during sepsis. The present health economic study shows that manage sepsis related tachyarrhythmia with landiolol is highly cost-effective and generates cost savings. Compared to SoC, landiolol yields cost savings of about 2,834 € from the German health care systems perspective and 1,380 € from the hospital perspective. The landiolol strategy, marked as “Dominant”, shows it saves money and improves outcomes compared to SOC. Total savings offset medication costs for landiolol of 1.156,00 €.
The following limitations should be considered when interpreting the results of the present analysis. First, the available clinical J-Land 3S trial was conducted in Japan, including only 150 patients. Due to that fact the AF protecting effect was subject of the sensitivitiy analysis. Furthermore, clinical data for long term outcomes associated with adverse effects and longterm sequelae are not available from the clinical J-Land 3S trial. Hence, the current model utilized an approach which assumes an overall decrease in lifeexpectancy associated with septic-shock survivors, with taking into account the potential effects of AF as long-term sequelae based on data published in the literature. Second, the clinical parameters were collected from randomized controlled trials, where care and monitoring may be more abundant than patients in a normal clinical setting. Third, only direct cost was captured in the economic evaluation. While indirect costs were not included, it is likely that survivors with long-term sequelae would have a greater loss of productivity.
The strength of the model is that the German clinical practice is depicted exactly, although RU data were taken from the J-Land 3S trial. The average hospital days of 26.4 and 26.2 respectively correspond to the average length of stay of the G-DRG flat rates used (between 8.6 and 32.3 days). Unit cost inputs represent prices and tariffs of the year 2020, no estimations were necessary. A life-time horizon was used to include the long-term follow-up, like the reduced life-expectancy associated with septic-shock survivors and the potential effects of AF as long-term sequelae. The model presented showed a substantial incremental gain in QALYs and reduction of costs for landiolol compared to SoC. Landiolol can therefore be considered as cost-saving in the management of sepsis related tachyarrhythmia.
This study was funded by a grant from Amomed Pharma GmbH, Austria.
E.W. previously received lecture fees from Amomed Pharma GmbH, Austria. G.K. is scientific advisor of AOP Gmbh., the registration holder of landiolol (Rapibloc).
E.W. has substantially contributed to the concept of the study, to the analysis and modelling and interpretation of the data, drafted the article, revised the article and finally approved the version to be published. G. K. initiated the study, revised the article and finally approved the version to be published.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Pharmacoeconomics: Open Access received 106 citations as per Google Scholar report