Research Article - (2022) Volume 10, Issue 6
Received: 24-Jun-2022, Manuscript No. jbhe-22-67661;
Editor assigned: 29-Jun-2022, Pre QC No. P-67661;
Reviewed: 04-Jul-2022, QC No. Q-67661;
Revised: 07-Jul-2022, Manuscript No. R-67661;
Published:
12-Jul-2022
, DOI: 10.37421/2380-5439.2022.10.100026
Citation: Nhial, Bang Chuol and Getahun Tadesse Haile. “Delivery Spacing and Associated Factors among Delivery Mothers in Gambella Region: A Facility Based Cross-sectional Study.” J Health Edu Res Dev 10 (2022):100026.
Copyright: © 2022 Nhial BC, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Background: Delivery spacing remains as one of the public health problems globally in general and developing countries in particular. Currently, little is known about the delivery spacing in the study area.
Objective: The aim of this study was to assess the delivery spacing and associated factors among delivery mothers in Gambella Region.
Methods: A facility based cross-sectional study was applied in Gambella region with the inclusion of one hundred and ninety six mothers in this study from February 1st, 2021 up to March 28th, 2021 while employing multi-stages sampling technique. Data were collected using structured interview. To ensure the quality of the data, a pretest of the tool, training of data collectors and field supervision were made. Using statistical package for social science version 25, median delivery spacing was computed and variables with p ≤ 0.20 from simple linear regression were declared as candidate for inclusion into multivariable analysis. Variables with p ≤ 0.05 from multivariable analysis were declared as factors significantly associated with the delivery spacing.
Results: The study resulted in 100% response rate. The median delivery spacing was found to be 34 months in the study area. Five factors such as; duration of breastfeeding (β=10.48, 95% CI: (8.50, 12.47)), maternal age (β=0.35, 95% CI: (0.10, 0.60)), maternal educational status (β=2.74, 95% CI: (0.70, 4.79)), partner educational status (β=3.12, 95% CI: (0.38, 5.87)) and mother occupational status (β=5.69, 95% CI: (3.81, 7.56)).
Conclusion and recommendation: In the study area, low median delivery spacing was found. Moreover, five factors like duration of breastfeeding, maternal age, maternal educational status, partner educational status and mother occupational status were found to be significantly associated with the delivery spacing. Based on the aforementioned conclusions, various recommendations were forwarded to the concerned bodies for the better response and for the request of conducting studies.s.
Delivery spacing • Delivery mothers • Gambella region
Background
Now a day, the delivery spacing (DS) has globally received much attention in the disciplines of demography and public health due to its crucial implication on the fertility and due to its provision of health benefits for not just the mothers but also the children later in life [1]. Women in developing countries have shorter delivery spacing than the recommended [2]. Africa is the leading continent in the world with the highest fertility rate (HFR) and the largest proportion of population growth [3]. According to World Health Organization (WHO), delivery spacing (DS) is defined as the time gap between two consecutive live births [4]. This delivery spacing is evidenced to be influenced by various factors among which postpartum amenorrhea and postpartum abstinence play significant role [5].
The WHO recommended that women should have at least 33 months to give birth and stay for at most 60 months (5 years) without giving birth. Short delivery spacing (SDS) and long delivery spacing (LDS) are time interval between two consecutive live births recommended by WHO to be at least 33 months and at most 60 months respectively. Both short and long delivery spacing are believed to have implication on maternal and child health [6,7].
Statement of the problem
Taking the global situation into focus, DS differs widely from certain country to country [8]. Worldwide, short delivery spacing of less than 24 months was estimated at 25% [9,10]. Among this proportion of short delivery spacing, an estimate of 33% and 20% were observed to be in Central Asia (CA) and Sub- Saharan Africa (SSA) respectively Tanzania, Uganda and Kenya had short delivery spacing of 19%, 25.9% and 18% respectively. The prevalence of short delivery spacing in Ethiopia was estimated to be in the range from 21.5% to 57.6% [11,12]. Evidences indicated that short delivery spacing is a cause of poor health outcome and that children whose mother experienced short delivery spacing are more likely to encounter certain health problems such as preterm, low birth weight (LBW), congenital malformation, early neonatal death and under five mortality later in life compared to those whose mothers did not [13,14]. In addition, short delivery spacing is a risk factor for maternal health and that mother who practiced short delivery spacing has more chance of the following health outcomes; third trimester bleeding, maternal mortality, blood pressure, anemia and pre-eclamsia compared to mother with delivery spacing of at least 33 moths [15].
Study area
This study was conducted in Gambella Regional State, a one of the ten regional states of Ethiopia found about 766 km away from Addis Ababa. It is found in South West of the country and bordered with the Oromiya Regional State in the East; with Benishangul-Gumuz Regional State in the North; with the Southern Nations Nationalities and People’s Regional State in the South and East; with the Republic of South Sudan in the West and North. On the basis of Ethiopia census conducted by Central Statistical Agency (CSA), the Gambela Region had an approximate population of 307,096, comprising of 159,787 males and 147,309 females with 14 woredas [16].
Study design and period
A facility based cross-sectional study design was conducted from February 1st, 2021 up to March 28th, 2021 in the selected health facilities in Gambella Region.
Source population
All mothers who delivered at health facilities in Gambella Region
Study population
All mothers who delivered in the selected health facilities in Gambella Region during the time of data collection.
Inclusion criterion
Mothers in each selected health facility in Gambella Region during the time of data collection was included in the study.
Exclusion criterion
Mothers who delivered for the first time.
Study variables
The dependent variable was the delivery spacing whereas independent variables include socio-demographic factors (maternal age, marital status, maternal educational status, partner educational status, maternal occupational status and partner occupational status maternal factors (gravidity and parity), delivery history related factors (no of children alive, sex of index child, pregnancy plan, ANC visits during index child pregnancy and mother decision making power) and obstetric related factors (duration of breast feeding, contraceptive use, survival status of index child awareness about the delivery spacing).
Sample size determination
The sample size was calculated using single population mean formula taking the following assumptions into consideration;
95% level of confidence,  1.96 with 5% margin of
error, σ=0.24
1.96 with 5% margin of
error, σ=0.24
Hence, 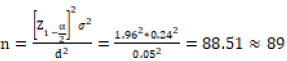 , adding 10% for possible
non-response rate and considering the design effect of 2, the sample size
becomes n = (89+9)*2=196 mothers.
, adding 10% for possible
non-response rate and considering the design effect of 2, the sample size
becomes n = (89+9)*2=196 mothers.
Sampling methods
A multi-stage sampling technique was employed during the selection of the district, health facilities and study respondents.
Data collection: Data were collected through face to face maternal interview. Data on socio-demographic, maternal, delivery history related and obstetric related factors of mothers were collected. Six data collectors and three supervisors who are health professionals were recruited as data collectors and supervisors respectively.
Data quality assurance: Questionnaire translation and review for the actual completion and the inclusion of all questions important for the objectives of the study were done prior to actual data gathering. The investigators were responsible for overall supervisions. Training was given to data collectors and supervisors. For further assurance of the data quality, pret-testing of the questionnaires were made in one health facility.
Data processing and management: Epi Info version 7 was used for data entry and transferred into statistical package for social science (SPSS) version 25 for analysis.
Data analysis: Descriptive and inferential statistics were performed. The descriptive statistics using measures of central tendency and dispersion (for continuous variables), tabular presentation using frequencies and proportions (for categorical variables) were done on one hand so as to estimate the median delivery spacing. Inferential statistics such as linear regression model was performed to identify the factors associated with the delivery spacing after reasonable assurance of the satisfaction of the assumptions of multiple linear regression model. Multivariable (multiple linear regression) analysis was computed after identified candidate variables for inclusion into multivariable analysis. Hence, the variables with p≤0.20 from bi-variable (simple linear regression) analysis were included into multivariable analysis so as to identify the factors significantly influencing the delivery spacing (having p≤0.05).
Ethical considerations
Ethical clearance was obtained from Ethic Review Committee (ERC) of Gambella University.
Following the endorsement by the ERC, all selected health facilities were informed about the objectives of the study through support letter from Gambella University. The purpose and importance of the study were explained to the study participants. After explanation, verbal consent was obtained from each study participant.
This study was conducted on 196 proposed respondents resulting in 100% response rate. One hundred and forty five (76%) of mothers are educated and fifty one (26%) of mothers are uneducated. One hundred and seventy three (88.3%) of partners are educated and twenty three (11.7%) of partners are uneducated.
Forty (20.4%) of mothers are employed and one hundred and fifty six (79.6%) of mothers are unemployed. The minimum and the maximum age of mothers are 22 and 42 years respectively with mean and standard deviation of 33.39 ± 5.07 years (Table 1).
| Variables | Category | Frequency | Percent |
|---|---|---|---|
| Marital status | Married | 190 | 96.9 |
| Single | 6 | 3.1 | |
| Maternal educational status | Educated | 145 | 74.0 |
| Uneducated | 51 | 26.0 | |
| Partner educational status | Educated | 173 | 88.3 |
| Uneducated | 23 | 11.7 | |
| Maternal occupational status | Employed | 40 | 20.4 |
| Unemployed | 156 | 79.6 | |
| Partner occupational status | Employed | 139 | 70.9 |
| Unemployed | 57 | 29.1 | |
| N | Min-Max | Mean ± SD | |
| Maternal age | 196 | 22-42 | 33.39 ± 5.07 |
Median delivery spacing
The median delivery spacing (MDS) in this study was estimated to be 34 months.
The delivery spacing will be 10.48 months higher for the mother who has breastfed her index child for at least 24 months compared to the mother who breastfed her index child less than 24 months when other factors are kept constant (β=10.48, 95% CI: (8.50, 12.47)). For one year increases in maternal age, the delivery spacing increases by 0.35 months when other factors remain unchanged (β=0.35, 95% CI: (0.10, 0.60)).
The delivery spacing increase by 2.74 months for educated mother compared to uneducated mother while keeping other factors constant (β=2.74, 95% CI: (0.70, 4.79)). The delivery spacing increases by 3.12 months for educated partner of the mother compared to uneducated partner of the mother while keeping other factors constant (β=3.12, 95% CI: (0.38, 5.87)). The delivery spacing will be 5.69 months higher for employed mother compared to unemployed mother while keeping other factors constant (β=5.69, 95% CI: (3.81, 7.56)) (Tables 2 -4)
| Variables | Category | Frequency | Percent |
|---|---|---|---|
| Sex of index child | Male | 120 | 61.2 |
| Female | 76 | 38.8 | |
| Pregnancy plan | Yes | 179 | 91.3 |
| No | 17 | 8.7 | |
| Antenatal care visits during index child | Yes | 122 | 62.2 |
| No | 74 | 37.8 | |
| Mother decision making power | Yes | 40 | 20.4 |
| No | 156 | 79.6 |
| Variables | Category | Frequency | Percent |
|---|---|---|---|
| Duration of breast feeding | >=24 | 118 | 60.2 |
| <24 | 78 | 39.8 | |
| Contraceptive use | Yes | 25 | 12.8 |
| No | 171 | 87.2 | |
| Survival status of index child | Alive | 186 | 94.9 |
| Not alive | 10 | 5.1 |
| Variables | Unstandardized Coefficients | Sig | 95% CI for B | ||
|---|---|---|---|---|---|
| B | Std. Error | Lower bound | Upper bound | ||
| Duration of breast feeding | 10.48 | 1.01 | p<0.001* | 8.50 | 12.47 |
| <24 months (Ref) | |||||
| Maternal age | 0.35 | 0.13 | 0.007* | 0.10 | 0.60 |
| Marital status | 2.39 | 2.14 | 0.267 | -1.85 | 6.61 |
| Single (Ref) | |||||
| Maternal educational status | 2.74 | 1.03 | 0.009* | 0.70 | 4.79 |
| Uneducated (Ref) | |||||
| Partner educational status | 3.12 | 1.39 | 0.026* | 0.38 | 5.87 |
| Uneducated (Ref) | |||||
| Maternal occupational status | 5.69 | 0.95 | p<0.001* | 3.81 | 7.56 |
| Unemployed (Ref) | |||||
| Partner occupational status | 0.97 | 1.12 | 0.386 | -3.18 | 1.23 |
| Unemployed (Ref) | |||||
| Gravidity | -0.45 | 0.96 | 0.636 | -2.34 | 1.44 |
| Parity | -1.09 | 1.51 | 0.471 | -4.07 | 1.89 |
| No of children alive | 1.23 | 1.12 | 0.272 | -0.97 | 3.44 |
| Sex of index child | 1.18 | 0.73 | 0.108 | -0.26 | 2.63 |
| Female (Ref) | |||||
| Pregnancy plan | 1.37 | 1.32 | 0.298 | -1.22 | 3.97 |
| No (Ref) | |||||
| Antenatal care visits during index child | -1.27 | 0.97 | 0.194 | -3.19 | 0.65 |
| No (Ref) | |||||
| Mother decision making power | -0.57 | 0.92 | 0.535 | -2.39 | 1.25 |
| No (Ref) | |||||
| Contraceptive use | 1.90 | 1.19 | 0.111 | -0.44 | 4.24 |
| No (Ref) | |||||
| Survival status of index child | 1.91 | 1.78 | 0.284 | -1.60 | 5.42 |
| Not alive (Ref) | |||||
Delivery spacing is believed to be one of the most important concepts that require much public health attention to be paid due to its various health benefits it provides.
The median delivery spacing in this study was found to be 34 months. The finding is consistent with the study done in Ethiopia using EDHS data with MDS of 32 months [17]. It is in line with study done in Southern Ethiopia with MDS of 33 months. Moreover, the finding is also consistent with the study done in Dedota, Arsi Zone with MDS of 32 months [18]. However, this finding is inconsistent with the study done in Bangladesh and the study done in Uganda with median delivery spacing of 55 and 22 months respectively. This inconsistency might be due to area and cultural difference of those countries with that of current study [15-19].
Maternal occupational status was found to be associated with the DS which is similar with the study done in Illubabor Zone in South West Ethiopia [20]. Furthermore, duration of breastfeeding was found to be associated with the DS in the current study and this is in line with the study done in Serbo of Jimma Zone [21]. In this study educational status of mother and partner were found to have significant influence on the DS and this finding is similar with the study done in Saudi Arabia [22]. Maternal age was found to be significantly associated with the DS in the current study which is consistent with the study done in Bangladesh.
Strength
Being initially conducted to consider the two directions of delivery spacing namely short and long delivery spacing is of great assistance to the science community. Data were gathered within 24 hours after birth which possibly may minimize the recall bias. The study resulted in 100% response rate which may maximize the precision of the estimate.
Despite its strengths, the study is conducted in the health facility alone in its scope excluding the home delivery mothers so generalization to all mothers in the area might be in doubt. Due to its cross-sectional study the seasonal variations might not be captured. Exclusion of environmental and cultural related factors might distort contextual understanding.
The median delivery spacing even if it fall within the recommended is still very low when considering at the aggregate level in the study area. Most of the mothers deliver shorter than the recommended which is believed to have contributed to short median delivery spacing. In the region, five factors were identified to be significantly associated with the delivery spacing namely; duration of breastfeeding, maternal age, maternal educational status, partner educational status and maternal occupational status.
Ethics approval and consent to participate
This study received ethics approval from Ethical Review Committee of Department of Public Health, Faculty of Natural and Computational Sciences, Gambella University (ID: DPH/001/022).
Consent for publication
All health facilities involved in this study were informed about the purpose of the study in local language appropriate for each, given opportunity to ask for clarity and their consents were received. Furthermore, all mothers participated in this study have given their consent.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
This study received fund from Gambella University.
BCN developed the proposal, designed the study and performed the statistical analysis. BCN and GTH monitored the data collection and drafted the final paper. GTH critically reviewed the paper, gave comments and advices. All authors read and approved the final manuscript.
We are so much grateful to Gambella University for the approval of the ethical clearance and for sponsoring the whole cost of this study. Furthermore, we would like to thanks all study participants, data collectors and supervisors for their exceptional contributions on this studys.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at