Research Article - (2023) Volume 8, Issue 6
Received: 21-Sep-2023, Manuscript No. jppr-23-114484;
Editor assigned: 25-Sep-2023, Pre QC No. P-114484;
Reviewed: 12-Oct-2023, QC No. Q-114484;
Revised: 26-Oct-2023, Manuscript No. R-114484;
Published:
02-Nov-2023
, DOI: 10.37421/2573-0312.2023.8.357
Citation: Siriguppa, Nihitha and B.N. Prem Kumar. “Effect of
Balance Exercises with Smart Phone Based Virtual Reality Programme on
Balance in Stroke Patients.” Physiother Rehabil 8 (2023): 357.
Copyright: © 2024 Siriguppa N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Background and objectives: Stroke is a neurological deficit, caused due to vascular changes. Impaired postural control and balance impairments in post stroke patients associated with high risk of fall among the stroke patients. The perturbation-based balance training is mainly used in older adults and balance impairment. Virtual Reality (VR) as a novel technology is rapidly becoming a popular intervention for improving balance. VR can visualize the computer- generated environments with full field of view by Head Mounted Displays (HMD-VR). This study was conducted to assess and investigate the effect of balance exercises with smart phone based virtual reality programme on balance in stroke patients.
Method: This was a randomized single-group pre and post-test study design. 30 subjects met the inclusion criteria and were enrolled, assigned and received intervention. Subjects were given perturbation based balance exercise and smart phone based virtual reality along with conventional physiotherapy. Intervention protocol was for 6 days/week for 4 weeks period.
Results: Following 4 weeks of intervention showed improvement in postural control and balance which was assessed using BBS, TUG, VR BESS, BESTest and SIS 3.0. Paired t test was used to differentiate the mean significance. The mean pre to post intervention difference is 12.6 with P value<0.05. TUG score improved from pre to post intervention difference is 1.443 with P value <0.05. VR BESS score improved from pre to post intervention difference is 10.266 with P value <0.05. The mean BESTest pre to post intervention difference is 11.467 with P value <0.05. SIS 3.0 score improved from pre to post intervention difference is 20.33 with P value<0.05. The result of this study showed highly significant difference in pre and post treatment.
Conclusion: The study concludes that perturbation based balance exercises with smart phone based virtual reality programme is a useful adjunct on improving balance in stroke patients along with conventional physiotherapy.
Postural control • Balance • Stroke • Perturbation based balance training • Smart phone based virtual reality • Virtual reality balance evaluation system test
ADL: Activities of Daily Living; BBS: Berg Balance Scale; BESTest: Balance Evaluation System Test; HO: Null Hypothesis; HMD: Head Mounted Device; Ha: Alternative Hypothesis; HRQoL: Health Related Quality of Life; MOCA: Montreal Cognitive Assessment; PBBT: Perturbation Based Balance Exercise; SPSS: Statistical Package of Social Sciences; SIS: Stroke Impact Scale; TUG: Timed Up and Go test; VR: Virtual Reality; VR BESS: Virtual Reality Balance Error Scoring System
Stroke is classically characterized as a neurological deficit and also neurological emergency attributed to an acute focal injury of the Central Nervous System (CNS) by a vascular cause [1,2], including cerebral infarction, Intracerebral Haemorrhage (ICH) and Subarachnoid Haemorrhage (SAH) and is a major cause of disability and death worldwide [3,4].
WHO definition of stroke (introduced in 1970 and still used) is “rapidly developing clinical signs of focal (or global) disturbance of cerebral function, lasting more than 24 hours or leading to death [5,6], with no apparent cause other than that of vascular origin [7]. The recommended standard WHO Stroke definition is “a focal or global neurological impairment of sudden onset and lasting more than 24 hours or leading to death and of presumed vascular origin” [8,9].
Clinical features as per vascular territory are as follows: In anterior cerebral artery infarct paresis or weakness of legs more than arm with sparing of hands, urinary incontinence, gait apraxia, akinetic mutism are seen [10]. In middle cerebral artery infarct homonymous hemianopia, aphasia (Broca’s and Wernicke’s), inattention, gaze paralysis, pareses of face-arm-leg are seen [11,12]. In vertebrobasilar artery infarct if occipital lobe is involved then symptoms like homonymous hemianopia, cortical blindness and other cortical visual deficits are seen [13]. If cerebellum is involved then ataxia, nystagmus is seen. If brainstem is involved then cranial nerve palsies with diplopia, vertigo, dysphagia, dysphonia is seen [14,15].
If spinal tract is involved hemiparesis and hemisensory loss are seen. In lacunar stroke syndromes (due to occlusion of deep perforating small arteries) symptoms like pure motor hemiparesis, pure sensory stroke, sensorimotor stroke, ataxic hemiparesis is seen [16,17].
Balance is the capability of maintaining the body’s centre of gravity within the base of support. Balance activity is mediated by three systems: biomechanical, neurological and sensory systems [18,19]. Motor, sensory and higher brain cognitive faculties to various degree, which leads to diminished balance, more postural sway, asymmetric weight distribution [20,21].
The novelty of perturbation training is in the focus on speed of processing and execution of limb movements [22,23], as well as rapid restabilization; this differs from ‘traditional’ balance training programs using voluntary movements that allow participants to control speed [24,25].
Virtual reality as a novel technology is rapidly becoming a popular intervention for improving balance and proliferated in the field of neurorehabilitation [26,27]. Interactive multimedia technologies offer certain advantages over traditional rehabilitation treatments either due to accessibility issues, geography or treatment availability, providing motivational activities, therapeutic adherence and treatment compliance [28,29]. Immersive VR we can visualize the computer - generated environments with full field of view by Head Mounted Displays (HMD-VR). This immersive virtual environment which represents as real environment can be used in balance training in which it continues visual feedback [30,31].
Virtual reality can be described in I3 terms:- INTERACTION+IMMERSION +IMAGINATION [32].
Conventional physical therapy based on activities of daily living skills include active assistive exercises for lower limb and upper limb, active exercises, functional retraining exercises, stretching, strengthening exercises, weight bearing exercises, weight shifting exercises, reaching exercises in sitting and standing, gait training [33,34].
Aim of the study
Aim of the study is to investigate the effect of balance exercises with smart phone based virtual reality programme on balance in stroke patients.
Research gap
There is no gap in knowledge or understanding of a subject. There is no lack of understanding of mechanisms behind disease and technology works.
Hypothesis
Null hypothesis: There may be no significant effects of balance exercises with smart phone based virtual reality programme on balance in stroke.
Alternate hypothesis: There may be significant effects of balance exercises with smart phone based virtual reality programme on balance in stroke.
Hence we accept alternative hypothesis and reject null hypothesis
The purpose of the study is to investigate the effect of balance exercises with smart phone based virtual reality programme on balance in stroke patients.
Method of collection of data
Study design: Randomized single- group pre and post - test study design.
Sample size: 30
Sample design: Purposive sampling
Study duration: 12 months
Source of data
• Out-patient department and in-patient department of General Medicine in Kempegowda Institute of medical sciences hospital and research centre, Bengaluru.
• Out-patient department of physiotherapy in Kempegowda Institute of medical sciences hospital and research centre, Bengaluru.
• Out-patient department and inpatient department of neurology, neurosurgery in Kempegowda institute of medical science hospital and research centre, Bengaluru.
Sample size estimation
• Sample size of unknown population-SSukp
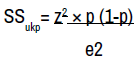
• z value - cumulative normal frequency, z= 1.96
• p - power of confidence
• e - margin of error= 0.05 (type I error)
• Here, p = 95% i.e., 0.05
So
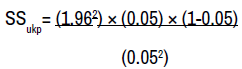
= 1.96 × 1.96 × 0.05 × 380 = 72.990
• SSukp = 245.6
• Sample size of known population - SSkp
SSkp= SSukp
1+ (SSukp/N)
• Here, N = Total number of patients per month= 2.5
SSkp = 72.990 = 1+(72.990/2.5) = 2.417
• SSkp which is approximately equal to 5 Therefore, SSkp=2.5 for one month
• Here, the study duration is 1 year (12 months) so, sample size=12 × 2.417=29.004 ≈ 30
• Therefore, total sample size = 30
Selection criteria
Inclusion criteria:
• Patients with Ischemic stroke diagnosed with a CT scan.
• Stroke within 45 days.
• A score of 26 points or higher of the Montreal cognitive assessment
• Both genders included.
• Subjects who are willing to participate, who have been explained and signed the written informed consent.
Exclusion criteria:
• Subjects with Perceptual cognitive deficits like hemi spatial neglect, attention and memory deficit.
• Subjects with Spinal and lower extremity deformity
• Subjects with Terminal illness or medically unstable
Materials used
• Smart phone
• Virtual reality- IRUSU MINI
• IN CELL (game app)
• Firm mattress
• Foam mattress
• Stop watch
• Measuring tape
• Arm rest Chair
• Cones / markers
The subject included will be explained about the intervention in the language understood by the subject / family members. A signed informed consent will be obtained in subjects/family own understandable language (Figure 1).
Data analysis
Descriptive and inferential statistical analysis has been carried out in the present study. Results on continuous measurements are presented on Mean ± SD (Min-Max) and results on categorical measurements are presented in Number (%). Significance is assessed at 5% level of significance (Table 1).
| Sl.no | Age | Gender | Berg Balance Scale (BBS) | Timed Up and Go Test (TUG) | Virtual Reality Balance Error Scoring System (VR-BESS) | Balance Evaluation System Test (BESTEST) | Stroke Impact Scale (SIS 3.0) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Day 1 | Day 4th week | Day 1 | Day 4th week | Day 1 | Day 4th week | Day 1 | Day 4th week | Day 1 | Day 4th week | |||
| 1 | 51 | Male | 31 | 48 | 13 | 10.93 | 31 | 20 | 80 | 93 | 30% | 75% |
| 2 | 55 | Male | 26 | 44 | 16.8 | 13 | 29 | 11 | 69 | 84 | 60% | 75% |
| 3 | 43 | Male | 36 | 45 | 12.14 | 17 | 30 | 19 | 75 | 83 | 75% | 80% |
| 4 | 66 | Male | 24 | 40 | 16 | 13 | 32 | 26 | 69 | 77 | 60% | 75% |
| 5 | 50 | Male | 33 | 43 | 17.12 | 13 | 33 | 29 | 64 | 76 | 40% | 65% |
| 6 | 55 | Male | 49 | 54 | 16.12 | 12 | 36 | 26 | 58 | 73 | 50% | 75% |
| 7 | 50 | Female | 36 | 45 | 12.14 | 17 | 30 | 19 | 75 | 83 | 75% | 80% |
| 8 | 66 | Male | 24 | 40 | 16 | 13 | 32 | 26 | 69 | 77 | 60% | 75% |
| 9 | 67 | Male | 36 | 45 | 12.14 | 17 | 30 | 19 | 75 | 83 | 75% | 80% |
| 10 | 74 | Female | 36 | 45 | 12.14 | 17 | 30 | 19 | 75 | 83 | 75% | 80% |
| 11 | 55 | Male | 26 | 44 | 16.8 | 13 | 29 | 11 | 69 | 84 | 60% | 75% |
| 12 | 75 | Male | 36 | 45 | 12.14 | 17 | 30 | 19 | 75 | 83 | 75% | 80% |
| 13 | 60 | Female | 36 | 45 | 12.14 | 17 | 30 | 19 | 75 | 83 | 75% | 80% |
| 14 | 66 | Male | 24 | 40 | 16 | 13 | 32 | 26 | 69 | 77 | 60% | 75% |
| 15 | 42 | Male | 36 | 45 | 12.14 | 17 | 30 | 19 | 75 | 83 | 75% | 80% |
| 16 | 51 | Male | 31 | 48 | 13 | 10.93 | 31 | 20 | 80 | 93 | 30% | 75% |
| 17 | 55 | Male | 26 | 44 | 16.8 | 13 | 29 | 11 | 69 | 84 | 60% | 75% |
| 18 | 50 | Male | 33 | 43 | 17.12 | 13 | 33 | 29 | 64 | 76 | 40% | 65% |
| 19 | 55 | Male | 49 | 54 | 16.12 | 12 | 36 | 26 | 58 | 73 | 50% | 75% |
| 20 | 51 | Male | 31 | 48 | 13 | 10.93 | 31 | 20 | 80 | 93 | 30% | 75% |
| 21 | 66 | Male | 24 | 40 | 16 | 13 | 32 | 26 | 69 | 77 | 60% | 75% |
| 22 | 50 | Male | 33 | 43 | 17.12 | 13 | 33 | 29 | 64 | 76 | 40% | 65% |
| 23 | 55 | Male | 49 | 54 | 16.12 | 12 | 36 | 26 | 58 | 73 | 50% | 75% |
| 24 | 51 | Male | 31 | 48 | 13 | 10.93 | 31 | 20 | 80 | 93 | 30% | 75% |
| 25 | 55 | Male | 26 | 44 | 16.8 | 13 | 29 | 11 | 69 | 84 | 60% | 75% |
| 26 | 50 | Male | 33 | 43 | 17.12 | 13 | 33 | 29 | 64 | 76 | 40% | 65% |
| 27 | 55 | Male | 49 | 54 | 16.12 | 12 | 36 | 26 | 58 | 73 | 50% | 75% |
| 28 | 51 | Male | 31 | 48 | 13 | 10.93 | 31 | 20 | 80 | 93 | 30% | 75% |
| 29 | 55 | Male | 26 | 44 | 16.8 | 13 | 29 | 11 | 69 | 84 | 60% | 75% |
| 30 | 66 | Male | 24 | 40 | 16 | 13 | 32 | 26 | 69 | 77 | 60% | 75% |
The following are the assumptions of the data;
• Dependent variables should be normally distributed,
• Samples drawn from the population should be random; Cases of the samples should be independent.
Statistical software: The Statistical software namely SPSS is used for the analysis of the data and Microsoft word and Excel have been used to generate graphs, tables etc.
Outcome measures
The Montreal Cognitive Assessment (MoCA) is a tool that can be used to systematically and thoroughly assess cognitive and mental status. It is a 1-page, 30-point test, administrable in ≈10minutes, which evaluates different domains: visuospatial abilities, executive functions, short-term memory recall, attention, concentration, working memory, language and orientation to time and space. The total possible score is 30, a score of 26 or above is considered as normal.
The Berg Balance Scale (BBS) was originally designed to quantitatively assess balance. The BBS is a 14 items scale that quantitatively assesses balance and risk for falls [35,36]. The scale requires 10 to 20 minutes to complete and measures the patient’s ability to maintain balance either statically or while performing various functional movements- for a specified duration of time. The BBS measures both static and dynamic aspects of balance [37,38].
The Timed up and Go test (TUG) is an objective clinical measure for assessing functional mobility and balance and thus the risk of falling [39,40]. The TUG measures the time taken for an individual to rise from chair, walk 3 meters, turn walk back and sit down using regular footwear and a walking aid if required [41,42]. Subjects are asked to stand up from a standard chair with a height of between 40 and 50 cm, walk a 3m distance at a normal pace, turn, walk back to the chair and sit down [43,44].
The Virtual Reality Balance Error Scoring System (VR-BESS) has improved the capability to detect lingering neurological and balance deficits [45,46]. This involved 3 minutes of sitting followed by 3 minutes of standing while wearing the VR headset and experiencing the rollercoaster stimulus attempting to maintain balance in two-leg, single-leg, or tandem stance on both foam and firm surface for 20 seconds in each stance (Figure 2).
The Balance Evaluation System Test (BESTest) is a new tool that assesses different balance systems including biomechanical constraints, stability limits/ verticality, anticipatory postural adjustments, postural responses, sensory orientation and gait stability [47,48]. It is divided into 27 tasks and 6 subgroups, each item is scored on a 4-level, ordinal scale from 0 (worst performance) to 3 (best performance). The total score for the test is 108 points.
The Stroke Impact Scale (SIS) 3.0 assesses 59 items of a patient’s quality of life, divided into eight dimensions where a stroke has an overall effect on health and well-being [49,50]. After SIS is administered, the respondent is asked to rate their percent recovery since their stroke on visual analogue scale of 0 to 100 with 0 meaning no recovery & 100 meaning full recovery.
Intervention
Perturbation based balance training:
• Perturbations were given in the sitting position on a couch and standing positions, with 10 sec hold, 10 perturbations in each position, 5 minutes.
• Perturbations were given in both right and left sideways forward and backward directions in sitting and standing.
• Perturbations were given at the shoulder, trunk and waist region (Figure 3).
Smartphone based virtual reality training:
• The therapist explains the neurorehabilitation program based on perturbation based balance exercise with head mounted display virtual reality (IRUSU MINI) with smart phone enclosed in it with the game “IN CEEL VR” and demonstrates the game through showing screen recording how to play (Figure 4).
• IN CELL VR game is an action racing VR game with a bit of strategy and science thrown into the mix. It will take an exciting journey inside the highly unusual micro world of human cell and stop the virus advance [51,52].
• IN CELL VR game that has specific tasks like hitting the proteins and avoiding the viruses. The subject had to hit the protein and avoiding the viruses, which is done in standing position [53].
Interpretations
Above table and graphs shows the mean and standard deviation of age. Subjects studied as mean of 56.367 and standard deviation of 8.29 (Table 2) (Figure 5).
| Missing | 0 |
| Mean | 56.367 |
| Standard Deviation | 8.2982 |
| Range | 33 |
| Minimum | 42 |
| Maximum | 75 |
Interpretation: Using t-statistics and a 5% level of significance. The critical value for the test with df=29 and alpha=0.05 is 2.045 and the decision rule is to reject null if the t-value is greater than are equal to 2.045. i.e., calculated value ≥ critical value.
• Calculated value = 14.586 and critical value=2.045.
• Hence, we reject null (H0) because 14.586 ≥ 2.045 and p<0.05. We have statistically significant evidence at alpha=0.05 to show there is a difference in the mean of the Berg Balance Scale on day 1 and the day 4th week.
• The result showed a significant difference in Berg balance scale scores within the group (p=0.00). Hence, we reject the null hypothesis and accept the alternative hypothesis that smart phone based virtual reality balance training with perturbation based balance training has a significant effect on stroke (Table 3).
| Variables | Mean | Std. Deviation | |
|---|---|---|---|
| BBS | Pre-score | 32.833 | 7.7819 |
| Post-score | 45.433 | 4.191 | |
| Difference | 12.6 | 3.5909 | |
| P value (within the group) - paired t test | <0.05** (t= -14.586) |
Interpretation: Using t-statistics and a 5% level of significance. The critical value for the test with degree of freedom=29 and alpha=0.05 is 2.045 and the decision rule is to Reject null if the t-value is greater than are equal to 2.045. i.e., calculated value ≥ critical value.
• Calculated value = 2.191 and critical value = 2.045.
• Hence, we reject null (H0) because 2.191 ≥ 2.045 and p<0.05. We have statistically significant evidence at alpha=0.05 to show there is a difference in the mean of the Timed up and Go test on day 1 and the day 4th week.
• The result showed a significant difference in Timed up and go test scores within the group (p=0.037). Hence, we reject the null hypothesis and accept the alternative hypothesis smart phone based virtual reality balance training with perturbation based balance training has a significant effect on stroke (Table 4).
| Variables | Mean | Std. Deviation | |
|---|---|---|---|
| TUG | Pre-score | 14.898 | 2.04383 |
| Post-score | 13.455 | 2.12711 | |
| Difference | 1.443 | 0.08328 | |
| P value (within the group) - paired t test | <0.05** (t=2.191) | ||
Interpretation: Using t-statistics and a 5% level of significance. The critical value for the test with degree of freedom=29 and alpha=0.05 is 2.045 and the decision rule is to Reject null if the t-value is greater than are equal to 2.045. i.e., calculated value ≥ critical value.
• Calculated value=12.867 and critical value=2.045.
• Hence, we reject null (H0) because 12.867 ≥ 2.045and p<0.05. We have statistically significant evidence at alpha=0.05 to show there is a difference in the mean of the virtual reality balance error scoring system on day 1 and the day 4th week.
• The result showed a significant difference in Virtual reality balance error scoring system scores within the group (p=0.00). Hence, we reject the null hypothesis and accept the alternative hypothesis that smart phone based virtual reality balance training with perturbation based balance training has a significant effect on stroke (Table 5).
| Variables | Mean | Std. Deviation | |
|---|---|---|---|
| VR BESS | Pre-score | 31.533 | 2.193 |
| Post-score | 21.267 | 5.9069 | |
| Difference | 10.266 | 3.7139 | |
| P value (within the group) - paired t test | <0.05** (t=12.867) | ||
Interpretation: Using t-statistics and a 5% level of significance. The critical value for the test with df=29 and alpha=0.05 is 2.045 and the decision rule is to Reject null if the t-value is greater than are equal to 2.045. i.e., calculated value ≥ critical value.
• Calculated value = 20.604 and critical value=2.045.
• Hence, we reject null (H0) because 20.604≥ 2.045and p<0.05. We have statistically significant evidence at alpha=0.05 to show there is a difference in the mean of the Balance evaluation system test on day 1 and the day 4th week.
• The result showed a significant difference in Balance evaluation system Test scores within the group (p=0.00). Hence, we reject the null hypothesis and accept the alternative hypothesis that smart phone based virtual reality training with perturbation based balance training has a significant effect on stroke (Table 6).
| Variables | Mean | Std. Deviation | |
|---|---|---|---|
| BEST TEST | Pre-score | 70.1 | 6.9597 |
| Post-score | 81.567 | 6.4844 | |
| Difference | 11.467 | 0.4753 | |
| P value (within the group) - paired t test | <0.05** (t=-20.604) | ||
Interpretation: Using t-statistics and a 5% level of significance. The critical value for the test with degree of freedom=29 and alpha=0.05 is 2.045 and the decision rule is to Reject null if the t-value is greater than are equal to 2.045. i.e., calculated value ≥ critical value.
• Calculated value=8.36 and critical value=2.045.
• Hence, we reject null (H0) because 8.36 ≥ 2.045and p<0.05. We have statistically significant evidence at alpha=0.05 to show there is a difference in the mean of the Stroke impact on day 1 and the day 4th week.
• The result showed a significant difference in SIS scores within the group (p=0.00). Hence, we reject the null hypothesis and accept the alternative hypothesis that smart phone based virtual reality balance training with perturbation based balance training has a significant effect on stroke (Table 7).
| Variables | Mean | Std. Deviation | |
|---|---|---|---|
| SIS | Pre-score | 54.50% | 15.72% |
| Post-score | 74.83% | 4.45% | |
| Difference | 20.33 | 11.27 | |
| P value (within group) - paired t test | <0.05** (t=-8.36) | ||
Limitations of the study
• Sample size was small, limited the generalizability of the results.
• The age group was kept wide due to unavailability of sample size.
• Only sub-acute stroke patients were included.
• Study duration was short i.e., only for 4 weeks.
• The study analysed only the short term benefits with respect to mobility, balance and function only.
Future scope and suggestions
• Future clinical trial study can be carried out on a large sample size.
• A similar study can be conducted in patients with different neurological conditions like Parkinson’s, cerebral palsy.
• In present study improvement in balance, postural control was seen in sub-acute stroke patients, so future study can also be done to see the effect of perturbation based balance training on all phases of stroke patients i.e., in acute and chronic.
• Further studies are needed to investigate the long term effects of mobile based virtual reality programme along with conventional physiotherapy treatment on balance, postural control.
Stroke is the leading cause of disability and frequent falling is one of the complications of post stroke. Impaired postural control and balance is associated with high incidence of falling in stroke. Incidence of fall in stroke, hence balance exercises are essential.
This study was conducted to find the effect of perturbation based balance exercise with smart phone based virtual reality along with conventional physiotherapy. After four weeks of intervention, Berg Balance Scale (BBS), Timed up and Go test (TUG), Virtual Reality Balance Error Scoring System (VR BESS), Balance Evaluation System Test (BESTest), Stroke Impact Scale 3.0 (SIS 3.0) were used to analyze the data, results of data analysis showed significant improvement in lower extremity function, balance, gait speed, functional ability, postural stability, muscular coordination, mobility and fall risk.
The findings provide a new paradigm of training guidelines for balance control and can reduce the risk of falling. This perturbation based balance training with smart phone based virtual reality program appears to be feasible and effective for improving balance after ischemic stroke. The findings from our study are clinically important, as they provide an innovative method for the treatment of stroke patients with an efficient, safe and low-cost program.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at