Research Article - (2024) Volume 14, Issue 4
Received: 19-Jul-2024, Manuscript No. jbbs-24-142521;
Editor assigned: 22-Jul-2024, Pre QC No. P-142521;
Reviewed: 01-Aug-2024, QC No. Q-142521;
Revised: 08-Aug-2024, Manuscript No. R-142521;
Published:
15-Aug-2024
, DOI: 10.37421/2155-9538.2024.14.426
Citation: Purohit, Prashant and John R. LaCourse. “Impact
of Fatigue Levels and Bed Heights on Chest Compression Dynamics during
Neonatal Cardiopulmonary Resuscitation: Real-Time Analysis.” J Bioengineer &
Biomedical Sci 14 (2024): 426.
Copyright: © 2024 Purohit P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This research study's primary focus is to examine Neonatal Cardiopulmonary Resuscitation (NCPR) dynamics, particularly analyzing real-time Chest Compression (CC) dynamics. Specifically, the study evaluates the dynamics of CC depth, recoil, rhythm, force, bed height, hand position, and fatigue levels to improve the quality and delivery of CC.
In this investigation, various CC methods, including Two-Thumb (TT), Two-Finger (TF), and Cross Four-Finger (CFF), were employed to perform CC at three different bed heights: normal, extended, and short. The impact of these various methods and bed heights on fatigue levels and the quality of CC is thoroughly examined and analyzed.
Furthermore, the study introduces a real-time fatigue level predicting method, which has been developed to assess its influence on CC quality and its impact on medical practitioners. The predicting method was developed by evaluating three machine-learning algorithms: Convolutional Neural Network (CNN), Long Short-Term Memory (LSTM), and Artificial Neural Network (ANN). The results indicate that the Two-Thumb method at normal bed height is the most effective and efficient approach. Additionally, the real-time fatigue level predicting method demonstrates superior performance compared to human perception of fatigue.
Neonatal Cardiopulmonary Resuscitation (NCPR) • Chest Compression (CC) • Two-Thumb (TT), Two-Finger (TF) • Cross Four-Finger (CFF) • Convolutional Neural Network (CNN) • Long Short-Term Memory (LSTM) • Artificial Neural Network (ANN)
Despite the advancements in medical care, there is a consistent rise in neonatal mortality rates globally due to various factors impacting the quality of Neonatal Cardiopulmonary Resuscitation (NCPR) [1]. These factors include inadequate training among medical practitioners, varying Chest Compression (CC) techniques such as Two-Thumb (TT), Two-Finger (TF), Cross Four- Finger (CFF), and the influence of fatigue on practitioners performing CC. It's crucial to address these challenges to improve the quality of CC and combat the increasing neonatal mortality rates worldwide [2].
Practitioner fatigue during NCPR can compromise the quality of chest compressions [3]. The guidelines set forth by the American Heart Association (AHA) are clear: the rotation of medical practitioners every two minutes is crucial to uphold the standard of CC [4]. The recommended CC depth is one-third of the anteroposterior diameter of the chest which is 3.8 cm (1.49 inches) approximately, the recoil should be 100% after each compression, and the Compression Rate (CPR) is 120 events / min which is 90 compressions and 30 ventilations. Therefore, conducting an analysis of practitioner fatigue during CC performance is imperative.
A series of research studies have consistently pointed out a significant drop in CC depth before the recommended two minutes of NCPR are completed [5-7]. These findings underscore the critical role of research in understanding the impact of lack of training for practitioners performing CC.
Insights from human biomechanics in CC have yielded significant and promising findings. Moreover, the influence of different elbow angles, linked to bed height, on the fatigue level adds complexity to the issue. Research studies have demonstrated that bed height does impact the quality of CC [8,9]. These insights can steer the development of ergonomic strategies to optimize CC performance and alleviate practitioner fatigue, inspiring a new era of improved NCPR.
The research results demonstrate variations in bed heights, suggesting a potential correlation between biomechanics, bed height, and the efficacy of CC. This offers a promising and hopeful avenue for further exploration and the potential development of practical solutions to enhance CC quality and reduce practitioner fatigue, paving the way for a brighter future in neonatal care.
Comprehensive training for experienced and inexperienced medical practitioners is imperative to reduce neonatal mortality significantly. This training should incorporate a real-time visual feedback model, especially in developing countries [7].
This research study aims to develop and implement a real-time visual feedback training device for medical practitioners with the following contributions:
• A comparison of different CC methods and a thorough analysis of medical practitioners' performance based on the quality of CC dynamics in real-time.
• Real-time monitoring and assessment of dynamic fatigue levels based on time and non-uniformity of CC depth.
• Investigation of the impact of bed heights on CC quality and fatigue levels.
• Exploration of the impact of hand position on CC dynamics.
• Evaluation of the significance of real-time fatigue levels on the performance and well-being of medical practitioners.
This research study was approved by IRB (FY2022-410).
Experimental setup
The experimental setup, designed with precision in mind, utilized two triple-axis accelerometers (HiLetgo MPU9250) and force sensors (interlink FSR 401) to collect real-time raw acceleration and force data. The sample rate for collecting acceleration data was set at 12 Hz. The accelerometer sensors were strategically placed on the chest (a1) and on the back (a2) of the SimNewB mannequin (Laerdal). In contrast, the force sensors were attached to the mannequin's chest to calculate the force applied during CC. The microcontroller (ESP32) was meticulously programmed using Visual Studio Core to collect real-time sensor data, and wireless communication was used to transfer the real-time data to MATLAB for further analysis and plotting. The block diagram in Figure 1 illustrates the precision of our experimental setup.
Mathematical equations
The displacement was determined using accelerometers, and from there, the depth and recoil were calculated. Different machine learning algorithms, such as Convolutional Neural Networks (CNN), Long Short-Term Memory (LSTM), and Artificial Neural Networks (ANN), were employed to train a model to predict fatigue levels.
Acceleration to displacement
The methodology for calculating the CC depth and recoil using accelerometers was thorough and rigorous. It began with the performance of a double integration on the real-time acceleration data to derive the displacement, as detailed in equations (1) and (2). Specific filtering techniques were employed to address the initial error of accelerometers and the errors accumulated during double integration. A 3rd order Butterworth high pass filter was used to mitigate the initial error of accelerometers, while a 3rd order Butterworth bandpass filter was implemented to address the errors accumulated during double integration. This thorough approach ensured the accuracy and reliability of our results.
The displacement was determined using two accelerometers, and the final displacement was computed by subtracting the displacement obtained from the top accelerometer (d1) and the displacement obtained from the bottom accelerometer (d2).
A method based on detecting maximum and minimum peaks was employed to calculate the CC depth and recoil. In this approach, the maximum peak represented the depth, while the minimum peak indicated the recoil. This peak detection technique allowed for real-time calculation of CC depth and recoil.
Furthermore, two separate algorithms were developed to facilitate these calculations. The algorithm for calculating CC depth and recoil in real-time is visually presented in Figure 2.

d(t): displacement with respect to time; dt: time difference between two samples
Convolutional Neural Network (CNN)
Convolutional Neural Networks (CNNs), a specialized deep learning algorithm, were processed and assessed for intricate time-series data. The primary aim is to harness CNN's capabilities to develop a model that can effectively predict the level of fatigue (classification) and pinpoint the timing of fatigue occurrence (regression) [10].
Convolution operation:

I: input; K: filter; M, N: dimensions of the filter; i, j: indices of the output feature
ReLU activation:

Fully connected layer:

W: weight matrix; x: input vector; b: bias vector
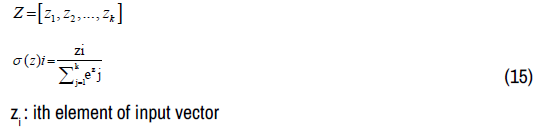
Classification output:

Training equations
Loss function for classification


Long Short-Term Memory (LSTM)
LSTM, which stands for Long-Short-Term Memory, is a special kind of Recurrent Neural Network (RNN) that solves the vanishing gradient problem in traditional RNNs. It can understand long term patterns in data by keeping track of information over time and selectively updating or forgetting information using gates [11].
Forget gate:
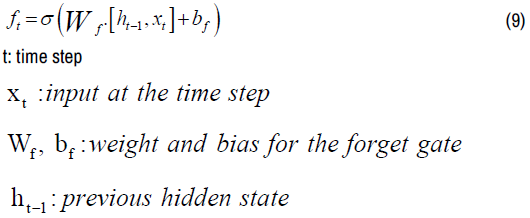
Input gate:

Candidate cell state:

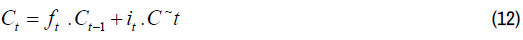
Update cell state:
Output gate:

Artificial Neural Network (ANN)
An artificial neural network is a computational model inspired by the structure and functions of the human brain. It is composed of interconnected nodes, called neurons, organized in layers. Information is processed and propagated through the network, starting from the input layer, then passing through intermediate hidden layers, and finally leading to the output layer. Each layer undertakes specific operations, such as data transformation, to contribute to the overall computation of the network [12].
Forward propagation:

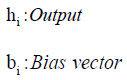
Output layer:
For classification:

For regression:
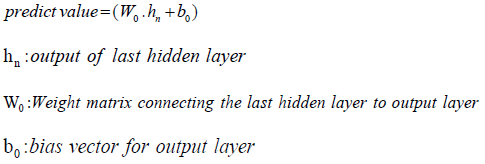
Softmax:
Input vector
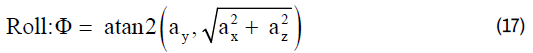
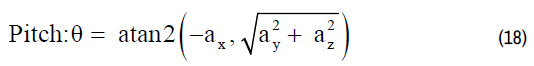
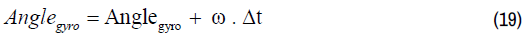
Complementary filter
The complementary filter, which combines acceleration and gyroscope data, was used to calculate an accurate and stable hand angle [13].
Complementary filter equation

Angle calculation using accelerometer data
Angle calculation using gyroscope data
This section discusses the results and statistical analysis to estimate the CC dynamics and compare different CC methods at discrete bed heights and their impact on CC and fatigue.
Chest compressions with and without visual feedback
In this pilot study, three medical practitioners conducted a comparative analysis of Chest Compressions (CC) with and without visual feedback to evaluate the impact of visual feedback on CC dynamics, precisely CC depth, recoil, and rate on the SimNewB manikin. The study utilized a paired t-test algorithm to compare the quality of CC depth when practitioners performed CC without and with visual feedback, using the parameters of TT, TF, and CFF at a normal bed height. The results of the analysis are presented in Table 1. Based on the paired t-test results, the p-value significantly varies in CC dynamics when performed with and without visual feedback. In this research, the p-values of mean depth, mean recoil and mean CC rate with and without visual feedback are 0.002, 0.002, and 0.001, respectively.
| NCPR dynamics | Non-feedback | Feedback | p-value |
|---|---|---|---|
| Mean CC Depth | 0.81 | 0.99 | 0.002 |
| Mean CC Recoil | 0.74 | 0.9 | 0.002 |
| Mean CC Rate | 196.8 | 110 | 0.001 |
CC dynamics and fatigue levels
The data was gathered in real time from five experienced medical practitioners who performed chest compressions on a SimNewB mannequin. Three different thresholds were examined to determine the optimum threshold for estimating dynamic fatigue levels compared to how humans perceive fatigue levels over time. The findings indicate that the mean time difference between Human Perception (HP) and Threshold 2 (T2) is the lowest at 29 seconds. In contrast, the mean time difference values between HP-T1 (Human perception – threshold 1) was 38.33 seconds, and HP-T3 (Human perception – threshold 3) was 68.33 seconds higher when compared with HP-T2. Additionally, Figure 3 visually compares the methods used to estimate the optimum threshold.
Machine learning algorithms
In this investigation, various machine learning algorithms were carefully examined to develop a cutting-edge real-time fatigue level prediction model to improve prediction accuracy significantly. It is important to note that machine learning algorithms are renowned for their flexibility, complexity, and ability to handle high-dimensional data [14]. Throughout the study, three advanced algorithms were tested: Convolutional Neural Network (CNN), Long Short-Term Memory (LSTM), and Artificial Neural Network (ANN). The resulting trained model was thoughtfully designed with two distinct layers, one for classifying fatigue levels and the other for accurately predicting the timing of each level [15-19].To assess and compare the performance of the three training models, the accuracy was carefully analyzed: Mean Squared Error (MSE), Root Mean Squared Error (RMSE), and Regression (R2). The comprehensive findings are presented in Table 2, providing a detailed comparison of the three models. Thorough analysis indicates that the LSTM training model is the optimal choice, as it achieved the lowest regression MSE and RMSE values and the highest R2 value. Furthermore, for a more comprehensive understanding, Figure 4 visually compares the three training models and offers valuable insights into their relative performances. Top left corner a) classification accuracy, top right corner b) MSE, bottom left corner c) RMSE, and bottom right corner d) R2. In this investigation, various machine learning algorithms were carefully examined to develop a cutting-edge real-time fatigue level prediction model to improve prediction accuracy significantly. It is important to note that machine learning algorithms are renowned for their flexibility, complexity, and ability to handle high-dimensional data [14]. Throughout the study, three advanced algorithms were tested: Convolutional Neural Network (CNN), Long Short-Term Memory (LSTM), and Artificial Neural Network (ANN). The resulting trained model was thoughtfully designed with two distinct layers, one for classifying fatigue levels and the other for accurately predicting the timing of each level [15-19].To assess and compare the performance of the three training models, the accuracy was carefully analyzed: Mean Squared Error (MSE), Root Mean Squared Error (RMSE), and regression (R2). The comprehensive findings are presented in Table 2, providing a detailed comparison of the three models. Thorough analysis indicates that the LSTM training model is the optimal choice, as it achieved the lowest regression MSE and RMSE values and the highest R2 value. Furthermore, for a more comprehensive understanding, Figure 4 visually compares the three training models and offers valuable insights into their relative performances. Top left corner a) classification accuracy, top right corner b) MSE, bottom left corner c) RMSE, and bottom right corner d) R2.
| Models | Classification Accuracy | Regression MSE |
Regression RMSE |
Regression R2 |
|---|---|---|---|---|
| CNN | 98% | 1.23 | 35.14 | 0.71 |
| LSTM | 98% | 1.13 | 33 | 0.74 |
| ANN | 98% | 1.18 | 34.46 | 0.71 |
Impact of CC methods on compression rate
It's essential to note the specified compression rate of 120 events per minute, comprising 90 compressions and 30 ventilations. In the context of this study, only compressions were performed. The Compression Rate (CR) is intricately linked to bed height and the duration of the activity. As time progresses, fatigue sets in, and the height of the bed significantly influences the effectiveness of Chest Compressions (CC). It's imperative to gain insights into how these factors impact the CR. Figure 5 visually represents the relationship between bed height, time, and the CR. Over time, the CR diminishes when CC is performed after one and two minutes at normal (TT_N) and extended bed heights (TT_E). Conversely, the CR rate increases at short bed heights (TT_S) after one and two minutes. Notably, the recommended CR was not attained at any bed height. Furthermore, the CR was lower when medical practitioners used the TF method than the TT method, specifically at discrete bed heights, particularly at 2 and 3 minutes. This disparity is depicted in Figures 6 and 7, which demonstrate the influence of bed height and time on CR using different methods.An interesting observation is that when medical practitioners performed CC at a short bed height using TT, TF, or CFF methods, the CR was higher after 2 minutes compared to the rates at normal and extended bed heights.
Fatigue level analysis
The study investigated the fatigue levels of individuals performing chest compressions (CC), focusing on how the bed height and technique influence these levels. We categorized the fatigue levels into three: low, moderate, and maximum fatigue, represented as 1, 2, and 3. The TT (Two-Thumb), TF (Two-Finger), and CFF (Cross-Four-Finger) methods were rigorously tested at normal, extended, and short bed heights. We compared three approaches to calculate fatigue levels and the time to reach them. As demonstrated in Figures 8-10, findings suggest that fatigue level calculations using LSTM (FLLSTM) closely correspond with the Fatigue Level of HP (FLHP) in comparison with Fatigue Level using Optimum Threshold (FLOT). Furthermore, it was found that using the TT method at normal bed height is significantly less fatiguing than using the TF or CFF methods at normal, extended, and short bed heights. This implies that medical practitioners could sustain chest compressions longer using the TT method at normal bed height.
Impact of CC methods and bed heights on CC force
The practitioners performed CC using TT, TF, and CFF at normal, extended, and short bed heights, and each method and bed height impacted the average force practitioners applied on the manikin’s chest while performing CC. Figure 11, represents the impact of discrete bed heights and CC methods on CC Force. The average force exerted on the manikin’s chest at normal bed height using TT, TF, and CFF is measured at 18 N, 12 N, and 14 N, respectively. At extended bed height, the average force applied using TT, TF, and CFF are 14N, 8N, and 10N, and at short bed height, the average force applied is 13N, 5N, and 8N, respectively. The average force applied to a manikin’s chest is comparatively lower at extended and short bed heights due to the extended or shortened position of the arms.
Impact of fatigue level on CC depth and recoil
The practical implications of this study's findings are significant. For instance, using the TT method for chest compressions led to a higher mean compression depth at fatigue level 1 compared to levels 2 and 3. Similarly, the mean compression depth at normal bed height was higher than that of extended and short bed heights. Moreover, approximately 84% of recoil was achieved with the TT method, as shown in Figure 12. These insights can help medical practitioners optimize chest compressions for improved patient outcomes, underscoring our research's relevance and potential impact.The analysis of chest compression performed using the TF method, considering the impact of fatigue level and different bed heights on compression depth and recoil, as illustrated in Figure 13, revealed superior mean compression depth at fatigue level 1 compared to extended and short bed heights. Moreover, mean depths were nearly identical when comparing extended and short bed heights at each fatigue level. Notably, substantial 93% recoil was attained using the TF method, further reinforcing the precision of our findings. This study also examined the CFF method, where the overall mean compression depth at different bed heights remained consistent across all fatigue levels. This suggests that bed height may not significantly impact compression depth when using the CFF method. Additionally, the CFF method yielded noteworthy 79% recoil, with normal bed height identified as optimal for recoil enhancement. As presented in Figure 14, these comprehensive results effectively capture the impact of bed height and fatigue on compression depth and recoil, further emphasizing the relevance of this research.
Impact of fatigue level on hand position
The fatigue experienced by practitioners during chest compressions significantly influences the positioning of their hands and, thus, the positioning of thumbs and fingers, subsequently affecting the depth and force of the compressions applied to the chest. [20-24]. Therefore, it is imperative to comprehensively understand and analyze the intricate nuances of hand positions at varying fatigue levels and operating at different bed heights while utilizing diverse compression methods. As illustrated in Figures 15-17, the impact of increasing fatigue levels on hand angle is discernible, ultimately reducing CC depth. The thumb and fingers are pronated or supinated with respect to the manikin’s chest. As the fatigue level increases, the mean hand angle increases, so a noticeable decrease appears in CC depth.
Impact of switching on CC
The research study involved two medical practitioners working collaboratively. One was administered chest compression (CC), while the other provided ventilation at the recommended rate provided by AHA. They alternated roles when the medical practitioner performing CC reached fatigue level 2. The study aimed to evaluate the impact of real-time dynamic fatigue levels on CC quality and enhance the practitioners' efficiency during practitioner’s rotation. The first medical practitioner performed CC at normal bed height using the TT method, and then they switched roles when the fatigue level reached 2 of the practitioners performing CC. Following the switch, the second practitioner continued with CC until reaching a fatigue level of 2, at this point, they switched roles again. Figure 18 compares the Human Perception (HP) and LSTM fatigue methods. According to the results, the LSTM fatigue method improved the efficiency of the medical practitioners, leading to increased fatigue time, mean depth, and mean force compared to the HP fatigue method.
In our insightful research study, we sought to explore the positive impact of real-time visual feedback on the depth, recoil, and rate of compressions performed by medical practitioners during NCPR. The findings highlight the constructive role that real-time visual feedback plays in enhancing the quality of CPR dynamics. Notably, a statistically significant difference in the p-values for compression depth (0.002) and recoil (0.001) when CPR is performed with real-time visual feedback even shows better results than those by Lin CY, et al. [2], Kim KH, et al. [25] and Wagner M, et al. [26] which emphasizes the constructive influence of this feedback mechanism on CPR performance.
This study measured the depth and recoil of Chest Compressions (CC) using different techniques (TT, TF, CFF) at normal bed height. The findings revealed that the average CC depth ranged from 1.06 cm to 0.97 cm, while the average recoil varied from -0.91 cm to -0.79 cm for the different techniques. Interestingly, it was noted that both the CC depth and recoil decreased when performed at extended and short bed heights.
When the bed is at a normal height, medical practitioners can maintain a neutral spine posture, effectively minimizing muscle stress and strain risk. However, practitioners would be forward flexion more when dealing with extended bed heights, adding stress to the back. This insight underscores the importance of considering bed height as a factor in reducing fatigue and preventing musculoskeletal strain among medical practitioners during patient care activities. This results in a reliance on the thumb and finger for force application rather than a combination of the arms, thumbs, and fingers as observed at normal bed height. Based on these findings, the most optimal method and bed height is Two-Thumb (TT) at normal bed height.
In the context of Chest Compressions (CC), it is imperative to consider the hand angle as a crucial factor in achieving the recommended depth with optimal force application. This research illuminates the impact of fatigue levels at varying bed heights, highlighting the nuanced changes in hand angle and subsequent reductions in mean depth at each fatigue level. Additionally, the study emphasizes the need to address the decrease in Compression Rates (CR) due to fatigue and the observable effects on CC depth and recoil. These insights pave the way for potential strategies to address fatigue-related challenges and improve performance in chest compression procedures.
An advanced Long Short-Term Memory (LSTM) innovative method was introduced in response to fatigue-related challenges. This innovative method harnesses predictive analytics to anticipate fatigue levels by analyzing critical factors such as Chest Compression (CC) depth and the duration of compression. After a comprehensive assessment, the LSTM innovative method was compared with the Human Perception (HP) fatigue method. The findings highlighted the remarkable superiority of the LSTM smart fatigue prediction method. Specifically, its implementation led to significant enhancements in CC quality, consequently contributing to a substantial improvement in the efficiency and performance of medical practitioners.
This research study made an intriguing discovery: when priority is given to achieving the recommended depth and recoil and using a less tiring method, the Compression Rate (CR) may be compromised. This raises an important discussion point for medical practitioners: Should they focus on maintaining the CR or prioritize achieving the recommended depth and recoil? This dilemma presents a significant consideration for those involved in clinical practice and highlights the need for further exploration and discussion within the medical community.
Real-time visual feedback has been demonstrated to enhance the dynamics and quality of Chest Compressions (CC) performed by healthcare professionals. Critical determinants impacting CC quality encompass bed height, CC technique, and practitioner fatigue. Notably, the preemptive assessment of fatigue levels and the rotation of medical personnel upon the onset of fatigue level two yield improvements in both CC quality and the overall efficiency of the practitioners in real-time.
One of the main challenges in CPR training is the size of the manikin used, which can limit its effectiveness. In addition, overestimating the recoil during chest compressions can lead to incorrect technique, making the training even more difficult.
Visual feedback that utilizes wearable technology to overcome these challenges is under development. It will be cost-effective and robust. Based on data from experienced medical practitioners, a standardized waveform will also be developed. With real-time visual feedback, this waveform can help achieve the recommended depth and recoil during chest compressions. Even the effect of fatigue on ventilation will be analyzed in future work.
None.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Journal of Bioengineering & Biomedical Science received 307 citations as per Google Scholar report