Research Article - (2022) Volume 6, Issue 3
Received: 02-May-2022, Manuscript No. jid-22-62490;
Editor assigned: 06-May-2022, Pre QC No. P-62490;
Reviewed: 18-May-2022, QC No. Q-62490;
Revised: 23-May-2022, Manuscript No. R-62490;
Published:
30-May-2022
, DOI: 10.37421/2684-4559.2022.6.171
Citation: Matakala, Mate. “The Prevalence of Tuberculosis and Associated Risk Factors in Twapia Area of Ndola District.” Clin Infect Dis 6 (2022): 171.
Copyright: © 2022 Matakala M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction: Globally, Tuberculosis is one of the most prevalent diseases which is mainly attributed to poverty and economic hardship, usually in developing countries. Knowledge of the current situation in our environment is necessary. The study on tuberculosis in Twapia has been carried out but with scant information on its prevalence. However, most of these studies were done prior to the introduction of the GeneXpert machines which is more accurate and sensitive for TB diagnosis as result studies to be done now with the new technology will yield more accurate results. Therefore, a study on the prevalence of TB in Twapia area of Ndola district is essential in order to fill in the gap knowledge, to understand if the TB cases are rising or reducing in number, to add on to the work done already, raise awareness and emphasis and ensure effectiveness in strategies to reduce the TB prevalence.
Aim: was to determine the prevalence of Tuberculosis (TB) and associated risk factor in Twapia area of Ndola district, particular patient seen by Twapia clinic.
Methodology: In this study a retrospective cross section study design was used, data was collected and sampled by complete enumeration of all TB patients’ files that visited Twapia clinic from January 2018 to December 2020. Out of a total of 49,820 patient’s files enrolled, 481 were diagnosed with TB. Data entry involved tabulations and use of SPSS software for analysis. All information collected was confidentially handled in accordance with the ethics. Ethical approval was obtained from Tropical Disease Research Centre (TDRC) and permission to conduct the study at the health institution was granted by both the Provincial Health Office and District Health Office.
Results: The prevalence of tuberculosis (TB) among Twapia residents was, according to these research findings, found to be increase from 2018 to 2020 as 25.2%, 34.5% and 40.3% respectively. It is densely distributed and more common between the ages of 36 to 45 years old. Of those who were treated for TB, it was found the majority were males representing 62.4% of the total cases. Those who had HIV/TB coinfection were 34.3% of the total cases treated for TB and the majority of cases were diagnosed using the GeneXpert.
Conclusion and recommendations: The prevalence of TB at Twapia clinic was found to be progressively increasing from 2018 at 25% to 40% in 2020, with the increase in prevalence, there is need to implement screening strategies, sensitize and encourage people to always visit hospital care and also to continue strengthening the DOT program. There is need to improve TB prophylaxis administration for those on ART and early diagnosis..
Background
Tuberculosis is a communicable chronic granulomatous disease caused by Mycobacterium tuberculosis. It usually involves the lungs but may affect any organ or tissue in the body. Tuberculosis flourishes under conditions of poverty, crowding, and chronic debilitating illness [1].
In 2017, TB caused an estimated 1.3 million deaths (range, 1.2–1.4 million) among HIV- negative people, and there were an additional 300 000 deaths from TB (range, 266 000– 335 000) among HIV-positive people. There were an estimated 10.0 million new cases of TB (range, 9.0–11.1 million), equivalent to 133 cases (range, 120–148) per 100 000 population affects all countries and all age groups, but overall the best estimates for 2017 were that 90% of cases were adults (aged ≥15 years), 64% were male, 9% were people living with HIV (72% of them in Africa) and two thirds were in eight countries: India (27%), China (9%), Indonesia (8%), the Philippines (6%), Pakistan (5%), Nigeria (4%), Bangladesh (4%) and South Africa (3%).Only 6% of cases were in the WHO European Region and the WHO Region of the Americas, each of which had 3% of cases. Zambia is a landlocked country which constitutes of 10 provinces with a population of 17 million people, it’s among the 30 high TB burden countries with TB incidence best estimate of 62 000, contributing 2.5% to the total TB incidence best estimate of Africa which is 2,480,000 (WHO, 2018).
The risk of progression from exposure to the tuberculosis bacilli to the development of active disease is a two stage process governed by both exogenous and endogenous risk factors. Exogenous factors play a key role in accentuating the progression from exposure to infection among which the bacillary load in the sputum and the proximity of an individual to an infectious TB case are key factors. Similarly, endogenous factors lead in progression from infection to active TB disease. Along with well-established risk factors (such as HIV, malnutrition, and young age), emerging variables such as diabetes, indoor air pollution, alcohol, use of immunosuppressive drugs, and tobacco smoke play a significant role at both the individual and population level. Socioeconomic and behavioral factors are also shown to increase the susceptibility to infection. Specific groups such as health care workers and indigenous population are also at an increased risk for TB infection and disease.
Tuberculosis (TB) and human immunodeficiency syndrome/acquired immunodeficiency syndrome (HIV/AIDS) constitute the main burden of infectious disease in resource limited countries. In the individual host, the two pathogens, Mycobacterium tuberculosis and HIV, potentiate one another, accelerating the deterioration of immunological functions. In high burden settlings, HIV coinfection is the most important risk factors for developing active TB, which increases the susceptibility to primary infection or reinfection and also the risk of TB reactivation for patients with latent TB.M. Tuberculosis infection also has a negative impact on the immune response to HIV, accelerating the progression from HIV infection to AIDS.
Zambia is ranked among the globe’s top 10 high TB incidence countries with an incidence rate of 280 smear positive tuberculosis (TB) cases per 100,000 inhabitants [2,3].
This research is focused on finding out the prevalence of TB in Twapia area in Ndola district of Copperbelt province despite measures put in place to reduce the disease burden. To achieve this, data will be collected at Ndola District health office. It’s important that this research is pursed so as to find better sustainable solution or improving and strengthening systems that are already there in reduction of TB burden as the nation pilgrimage towards attaining the third (3) sustainable development goal which is focused on ensuring healthy lives and promoting well-being for all ages. Leaving TB crisis unattended to can greatly impact the public health causing a rampant spread of the disease which has repo effect on the economy and manpower.
Problem Statement
Tuberculosis (TB) is a worldwide and one of the most important human bacterial diseases. Although rates of infection are now low in developed countries, HIV infected, homeless and malnourished people are highly susceptible, as are immigrants from areas where the disease is endemic.in some developing countries; the incidence reaches 450 per 100,000, with a high fatality rate [4,5].
Zambia has experienced a rapid increase in TB cases, simultaneously with the beginning of HIV era in 1983. The World Health Organization (WHO) estimates the prevalence of all forms of TB in Zambia at 707 per 100,000 and ranks Zambia as ninth in the world for TB incidence rate with an incidence of smear positive cases at 288 per 100,000. Ndola district is not exceptional from contribution to the TB burden in Zambia [6].
GeneXpert technique now serves as the cornerstone for diagnosis of TB in Ndola District. However, the prevalence of TB in Ndola District of Zambia, including Twapia area still remains unknown Studies done in Ndola district have scant information on the prevalence of TB instead, there are focused on transmission of TB, various strains of TB that are common, multidrug resistance TB among others. However, most of these studies were done prior to the introduction of the GeneXpert machines which is more accurate and sensitive for diagnosis. Data collected is more reliable and accurate as opposed to the previously used methods of diagnosis.
Therefore, this study aims at determining the prevalence of TB in Twapia area of Ndola district of Zambia in order to fill in the gap knowledge, to add on to the work done already, raise awareness and emphasis and ensure effectiveness in strategies to reduce the TB prevalence.
Justification of the Study
The study is important that it should be carried to find out the prevalence of TB in Twapia area of Ndola district because there is paucity of information on the prevalence of TB in the area despite it being the fourth largest ward, harboring a large population which is prone to tuberculosis (TB). The translational results generated study, will guild policy and help clinicians in the management of TB. It will also increase awareness on the prevalence of TB in Twapia which will be brought to the attention of various stakeholders and also contributing to the body of knowledge.
Worldwide, Tuberculosis (TB) is of the top 10 causes of death and the leading cause from a single infectious agent (above HIV/AIDS). Millions of people each continue to fall sick with tuberculosis. In 2014, 9.6 million people fell ill with TB including 1.2 million people living with HIV, 1.5 million people died from TB and 0.4 million among people with HIV.TB is one of the top five killer disease of adult women aged 20 to 59 years, 480 000 women died from TB and 140 000 among those who were HIV positive, atleast 1 million children became ill with TB and an estimated 140 000 children died from TB and 55 000 among those who were HIV positive. Over 3 million people who developed TB in 2014 were missed by national systems. (WHO, 2015)
After 2 decades of annual declines, TB incidence in the USA has leveled at approximately3.0 new cases per 100,000 persons. The determinant in the leveling of TB incidence is not yet clear. The preliminary data reported to the National Tuberculosis Surveillance System indicated TB incidence among foreign born persons in the USA (15.1 cases per 100,000) has remained approximately 13 times the incidence among US born persons (1.2 cases per 100,000). Among the 9,563 TB cases reported during 2015, 13 201(33.5%) occurred among the US born persons corresponding to an annual TB incidence of 1.2 per persons. The 6,335 TB cases among foreign born in the USA (66.2%) of the total US cases) corresponded to an annual TB incidence of 15.1 per 100,000 persons. TB incidence among the US foreign born persons has continued to decline, in contrast, stabilization of TB incidence among the US born persons evidenced by molecular genotyping of TB cases demonstrates TB transmission still occurring. Therefore, effective control by early case diagnosis, timely diagnosis and treatment completion [5].
Another publication by Van Der Werf and Zellwerger of 2016 explains that European Union (EU)/European Economic Area (EEA) countries have witnessed an unprecedented volume of migration, with 1,046,599 migrants arriving in Europe most of which are Syrian, Iraq nationality or afghan via the route of the eastern Mediterranean. These migrations have been implicated in the transmission of TB.in 2013, 3.3% of all TB cases notified in the EU/EEA originated from other EU/EEA countries and more than 60% of those originated from Poland and Romania. The latest TB surveillance data report Published by the WHO regional office for Europe and the European center for disease prevention and control on the occasion of world TB day 2016, shows that in 2014, 58008 TB cases were reported by 29 EU/EEA countries notification rate of 12.8 TB cases per 100,000 populations. In support of this Kodmon, et al. acknowledges the important and increasing contribution of migration from high incidence countries outside the EU/EEA to the epidemiology of TB in Europe. What has been shown is that TB rates often remain high in migrant populations. Therefore, screening upon entry into the host country may be considered though it is an option that is implemented by some EU countries [7].
Furthermore, a study carried out in India shows that one fourth of the global incident tuberculosis (TB) cases occur in India annually. In 2012 out of the estimated global annual incidence of 8.6 million TB cases, 2.3 million were estimated to have occurred in India. TB is the seventh most common cause of mortality worldwide. A cross sectional questionnaire based epidemiology was conducted in 510 TB patients of age group 16 – 78 years for 9 months, it was found that apart from the multi-drug therapy, poor knowledge and awareness regarding TB among TB patients is alarming sign for the nation [8-10].
A similar study was done in Saudi Arabia using a cross – sectional survey of 1004 residents, spread of TB by coughing was a transmission route known by 44.2% of males and 59.6% of females, 12.0% participants knew TB is caused by bacteria, 71.1% of females and 52.3% males, knew TB is infectious. Overall, high number of participants not knowing anything were recorded, from these findings it was concluded that knowledge is lacking concerning TB transmission, the cause of disease, means of prevention and the success treatment, highlighting an urgent need for better public education [1].
However, the burden of tuberculosis in Zambia is among the highest in the African region and in 2013 the prevalence was estimated at 388/100,000 population according to WHO and estimated incidence rate of 427/100,000 population; TB is one of the major public health problems in the country with a notification rate of 289/100,000 population of all forms of TB in 2012. A first national TB prevalence survey was done as Zambia was one of the 22 high priority countries selected by WHO because it met the criteria as defined by The WHO Global Task Force on TB impact measurement. Having no background of any TB prevalence surveys, the country lacked baseline data on the prevalence TB, the WHO recommends implementation of population based-prevalence surveys to estimate the prevalence of TB baseline and consequently impact assessment to measure progress. Currently the country is relying on routine surveillance data from health facilities collected through national TB control targets despite these there are limitations with data collection [2].
Zambia continues to grapple with a high TB burden despite a long running Directly Observed Treatment Short course program. Understanding issues that affect patient adherence to treatment is an important implementation to a successful TB control agenda. A cross section study of 105 respondents was done, who had been registered as pulmonary TB patient (new and retreatment) in Ndola district between January 2006 and July 2007. A structured questionnaire was administered, bearing questions to obtain individual data on social demographic, health seeking behavior, knowledge on TB, reported adherence to TB treatment, and health center care received during treatment to consenting respondents.it was identified that respondents delayed to seek treatment (68%) even when knowledge of TB was high (78%) or when they suspected that they had TB (73%). Respondent adherence to taking medication was high (77%) but low adherence to submitting follow up sputum (47%) was observed in this group. Similarly, care givers educate their patient more often on the treatment of the disease (98%) and drug taking (100%), than on submitting sputum during treatment (53%) and its importance (54%). Respondents adherence to treatment was significantly associated with respondent’s knowledge about the disease and its treatment (p>0.0001), and with caregiver’s adherence to treatment guidelines (p=0.0027). There is need to emphasize the importance of submitting follow up sputum during patient education and counselling in order to enhance patient adherence and ultimately treatment outcome [4].
The Copper belt Province was responsible for nearly a third (27.6%) of the nation's notified TB cases. It was also one of the provinces with the highest Human Immunodeficiency Virus (HIV) prevalence (17%) in Zambia based on the National Tuberculosis Leprosy Program, in 2004 [6].
Tuberculosis (TB) incidence is increasing in much of sub-Saharan Africa, largely due to the high prevalence of HIV infection. International TB control strategies rely on self- presentation of cases to the health services, diagnosis by sputum smear microscopy and the use of a 6–8 month course of multi-drug therapy to cure the disease. However, these strategies are currently failing to control TB in high HIV prevalence settings, due both to the massive burden of disease and the inadequacy of existing health systems to find and cure infectious cases coupled with the continuing stigma and denial that surround HIV and TB.
Globally, the World Health Organization (WHO) reports an estimated prevalence of 3.6% and 20.2% among notified TB cases for primary and acquired multidrug resistant tuberculosis (MDR-TB), respectively, with significant country and regional variations. Despite the high burden of TB in sub-Saharan Africa (SSA) fueled by HIV, drug resistance surveillance has not been widely done, with only 22 of the 46 countries reporting drug resistance data by 2005 [11].
During the 1990s, multidrug-resistant tuberculosis (MDR-TB), defined as resistant to at least isoniazid and rifampin, emerged as a threat to TB control. Globally, 480,000 new TB cases (3.9%) are MDR-TB in 2015. In China, the proportion of MDR-TB cases is growing dramatically, and national survey estimated that there were 110,000 cases of MDR-TB and 8,200 cases of XDRTB [12-14]. Despite China having the second highest incidence of MDR-TB, information regarding MDR-TB and resistance to second-line anti tuberculosis drugs (SLDs) among MDR-TB isolates still remains unclear for many regions of China.
‘’Our population-based observational study demonstrated that 54.4% MDR-TB patients in Shanghai had already had resistance to at least one SLD, which was even worse than that in other reports in China (51.8%), India (44.8%), Russia (43.3%), and Poland (30.4%).’’ [15].
In Zambia, TB case notifications decreased from 48,616 in 2010 to 41,588 in 2015, while treatment success rates among patients with new sputum smear positive pulmonary TB stayed consistently at 785%. However, there has been increasing concern about MDR-TB. Zambia’s National TB and Leprosy Control Programme (NTLP) conducted a national drug Resistance survey in 2008 that showed that combined MDR-TB prevalence in new and previously treated patients varied between 1.1% and 1.6%, depending on the diagnostic method used. Since then, MDR-TB has increased, with an estimated prevalence of 3.7% of all cases in 2015 (1.1% among new cases and 18% among previously treated cases) [16].
Drug resistance is a severe challenge to tuberculosis control, as it raises the possibility of a condition that can no longer effectively be treated with antituberculosis drugs and further transmission to public population. This situation of MDR-TB highlights the urgent need for rapid and accurate drug susceptibility testing (DST) to optimize the treatment regimen and reduce the risk of acquired resistance.
Objectives
General objective: To determine the prevalence of tuberculosis in Twapia rural area in Ndola district of Copperbelt province by cases recorded at the district health office.
Specific objectives:
• To determine the proportion of TB cases in Twapia area of Ndola District.
• To evaluate the trend of TB in Twapia area of Ndola District.
• To determine factors associated with TB prevalence in Twapia.
Research question
What is the prevalence of TB in Twapia area of Ndola district of Zambia?
Measurement
Operational definitions
Prevalence: Measurement of all individuals affected by Mycobacterium tuberculosis at a particular time in Twapia area.
Proportion: Comparative relation of the magnitude as size, number etc. of TB cases in Twapia area.
Trend: the general direction in which TB cases in Twapia are developing or changing, either increasing or decreasing.
Study variables
Poverty: tuberculosis is a disease of poverty. It is widely recognized that the poorer the community, the greater the likelihood of being infected with the TB germ and developing clinical conditions. Fighting TB and poverty together is necessary to accelerate economic and social growth and consistently reduce the burden of TB. A lack of basic health services, poor nutrition and inadequate living conditions all contribute to the spread of TB and its impact upon the community. Overcrowded and poorly ventilated home and work environment make TB transmission more likely. Unemployment is an intervening variable for poverty and overcrowding.
HIV/AIDS: HIV weakens the immune system thus reducing its ability to fight the TB germ, increasing the risk of TB in people living with HIV. Latent TB is more likely to advance to TB disease in people with HIV.TB is one of the leading causes of death among people with HIV.
Age: tuberculosis mostly affects adults in their most productive age. However, all age groups are at risk.
Lack of education: low level of knowledge on TB can lead to complications and worse health outcomes increasing the transmission and delaying health seeking behaviour, lack of adherence, resulting in multidrug resistance, treatment failure, and disease complication and death.
Gender and Sex: However, several other, more specific biological sex related factors may render men even more susceptible to pulmonary TB than women; sex steroid hormones, the genetic makeup of the sex chromosomes, and sex specific metabolic features (Figure 1).
Study area
Ndola is the third largest city in Zambia. It is the industrial and commercial center of the Copper belt, Zambia’s copper mining region and a capital of Copper belt province. It has a population of 475, 194 (2010 census provisional). it lies between latitudes 120˚ and 160˚ South of the Equator and between 250˚ and 30˚ east. It has 31 health facilities: 28 primary health centers or clinics, 2 referral hospitals and 1 infectious disease reference laboratory. Most of these health Centre’s provide TB diagnosis and treatment. However, it is comprised of 28 wards among which Twapia being one of them. Twapia is the fourth largest ward with a population size of 26 683 (2010 census provisional). Data on TB cases reported from Twapia area was collected at Twapia clinic registers and Ndola District Health Office.
Study population
This included all TB cases reported by the Ndola District Health office and records at Twapia clinic registers, patient treated, relapse cases which can be primary (in a person who has had TB before) or secondary (in a person who has had TB Before), age groups, geographical origin, occupation and other epidemiological characteristics.
Study design
This was a descriptive retrospective study in which data on TB cases reported from Twapia area was collected from registers/information systems at Ndola District Health Office and Twapia clinic. This included data on TB cases reported from 2018 to 2020, and demographic data on the TB patients.
Sample size
A 50% prevalence rate was used to calculate the sample size using the formula below:
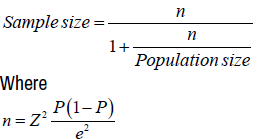
Calculations:
Where
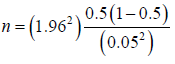

Sample size = 379
Calculated sample size is 379
Inclusion and exclusion criteria
The study involved TB cases diagnosed in Twapia area from 2018 to 2020 of adult patients (15years and above). All TB cases from children less 15years was excluded from the study.
Sampling
Systemic random sampling was used to obtain the desired sample size by using the registry at Twapia clinic and information system of Ndola district health office. A sampling frame comprising TB cases recorded from 2018 to 2020 was made.
Data collection
Data was collected from Twapia clinic and Ndola district health office which was utilized to meet the specific objectives of the study.
Data analysis
Data entry and analysis was done using trend analysis on the latest computer software SPSS, to generate the pattern and distribution by age and year within the stipulated time.
Ethical consideration
Ethical clearance was obtained from the Ethical Boards Tropical Diseases Research Center (TDRC) and The Copper belt University to ensure misconduct and violation of ethics is avoided. With respect to ethics, the research upheld confidentiality and informed consent. This was done by explaining the research and its purpose fully to the intended participants. Both advantages and disadvantages such as disturbances and discomfort that were to be felt and experienced during that time of retrieval of hospital file records. It was also explained to the person in charge of supervision in the process of data collection, that they were free to withdraw and report any misconduct, misuse or inappropriate use Clinical Records observed, if any was to be observed. Moreover, the research proposal was submitted to ethical board for scrutiny to ensure that sound ethical consideration is upheld before the research is carried out, and approval was given. Additionally, the information gathered is kept strictly confidential.
The aim of this research was to determine the prevalence, trend of tuberculosis and associated risk factor in Twapia, Seen at Twapia Clinic in Ndola.
The files that were available during data collection were files only from 2018 January to 2020 December 2020 and by Complete Enumeration of all available patient’s files with diagnosed tuberculosis, were files sampled.
Data analysis
Data for tuberculosis cases was collected from the Twapia Clinic Registry book, which captured patients from 2018 January to 2020 December by use of a structured data collection tool. Data was then later processed manually and entered on the data master sheet. This exercises included tables, frequency counts, percentages and comparison of variables. Cross tabulation of variables was done to show relationship among variables in numerical form.
Presentation of findings
The total number of patients that visited Twapia urban health center outpatient department (OPD) during the study period were 49,820,481 (0.97%) patients were diagnosed and treated for TB.
For this research, we define TB as to include those who were diagnosed clinically and bacteriologically.
Tuberculosis (TB) in this study represents 0.97% (481) of all patients that visited Twapia urban center outpatient department in Ndola in the period January 2018 to December 2020.
The prevalence of tuberculosis (TB) among Twapia residents was, according to these research findings, found to be increase from 2018 to 2020 as 25.2%, 34.5% and 40.3% respectively. Of those who were treated for TB, it was found the majority were males representing 62.4% of the total cases. Those who had HIV/TB coinfection were 34.3% of the total cases treated for TB and the majority of cases were diagnosed using the gene xpert.
This agrees with the study by Mulenga C, et al. [4] which stated that the Copperbelt Province was responsible for nearly a third (27.6%) of the nation's notified TB cases. It was also one of the provinces with the highest Human Immunodeficiency Virus (HIV) prevalence (17%) in Zambia based on the National Tuberculosis Leprosy Program, in 2004.
According to these findings, sex, age and HIV status have an impact on TB prevalence, this is in agreement with studies done in African countries on TB prevalence and its distribution pattern among sex, age and HIV patients [14-20].
It was noted that among the patients that were treated, there was no any case of treatment failure that was recorded which is attributed to good adherence and effectiveness of DOT. However, a few poor outcome was recorded 18 died, 7 were lost to follow and 3 defaulted.
The data as to whether poverty, education background and economic status highly contribute to one having TB cannot be concluded upon since we could not find sufficient data to help us reaffirm and conclude as such (Tables 1-11).
| Year | Month | No. months | Total OPD Cases |
|---|---|---|---|
| 2018 | January to December | 12 | 8,665 |
| 2019 | January to December | 12 | 19,704 |
| 2020 | January to December | 12 | 21,451 |
| Total number of | 36 Months | 49,820 Patients | |
| Year | Month | No. Months | Total TB cases |
|---|---|---|---|
| 2018 | January to December | 12 | 121 |
| 2019 | January to December | 12 | 166 |
| 2020 | January to December | 12 | 194 |
| Total Number of | 36 months | 481 patients | |
| Year | Frequency | Percentage (%) |
|---|---|---|
| 2018 | 121 | 25% |
| 2019 | 166 | 35% |
| 2020 | 194 | 40% |
| Total | 481 Patients | 100% |
| Bacteriologically | Clinically | |||
|---|---|---|---|---|
| Year | Gene x-pert | Sputum smear -afb | Culture | Chest X-ray |
| 2018 | 65 | 22 | 0 | 34 |
| 2019 | 93 | 37 | 0 | 36 |
| 2020 | 114 | 52 | 0 | 28 |
| Total | 273 | 111 | 0 | 98 |
| Year | Cured | Treatment Completed |
Died | Lost to Follow |
Treatment Failure |
Defaulter |
|---|---|---|---|---|---|---|
| 2018 | 59 | 50 | 5 | 6 | 0 | 1 |
| 2019 | 101 | 53 | 9 | 1 | 0 | 2 |
| 2020 | 103 | 87 | 4 | 0 | 0 | 0 |
| Total | 263 | 190 | 18 | 7 | 0 | 3 |
| Year | Number of Patient | Percentage |
|---|---|---|
| 2018 | 56 | 34% |
| 2019 | 64 | 39% |
| 2020 | 45 | 27% |
| Total | 165 | 100% |
| Tuberculosis (TB) Distribution By Age | ||
|---|---|---|
| Age Group | Number of Patients | Percentage |
| 15 -25 | 122 | 25.4% |
| 26-35 | 113 | 27.7% |
| 36-45 | 140 | 29.1% |
| >46 | 106 | 22% |
| Total | 481 | 100% |
| Year | Tuberculosis (tb) distribution by sex | |
|---|---|---|
| Male | Female | |
| 2018 | 77 | 44 |
| 2019 | 110 | 56 |
| 2020 | 113 | 81 |
| Total | 300 | 181 |
| Percentage | 62.4% | 37.6% |
| Year | |||
|---|---|---|---|
| Month | 2018 | 2019 | 2020 |
| January | 13 | 15 | 15 |
| February | 9 | 20 | 15 |
| March | 10 | 14 | 15 |
| April | 12 | 8 | 10 |
| May | 9 | 7 | 8 |
| June | 8 | 17 | 11 |
| July | 9 | 15 | 45 |
| August | 4 | 14 | 5 |
| September | 5 | 17 | 25 |
| October | 16 | 10 | 15 |
| November | 9 | 14 | 15 |
| December | 14 | 15 | 15 |
| Total | 121 | 166 | 194 |
| Activity | Unit Measure | Unit Price (K) | Quantity | Total Price (K) |
|---|---|---|---|---|
| Rim of paper | Each | 50.00 | 2 | 100.00 |
| Pens | Each | 2.50 | 5 | 12.50 |
| Pencils | Each | 2.00 | 2 | 4.00 |
| Eraser | Each | 2.50 | 2 | 5.00 |
| Typing proposal | Each page | 2.50 | 20 | 50.00 |
| Printing proposal | Each page | 2.50 | 20 | 50.00 |
| Transport allowance | - | - | 1 | 200.00 |
| Typing report | Each copy | 90.00 | 1 | 90.00 |
| Printing and binding report | Each copy | 120.00 | 2 | 240.00 |
| Assistants allowance | Each | 500.00 | 2 | 1,000.00 |
| Meal allowance | Each | 900.00 | 1 | 900.00 |
| Grand Total | - | - | - | 2651.50 |
| Task to be performed | January-to-April 2019 | January-to- February 2022 | January to march 2022 | May 2022 |
|---|---|---|---|---|
| Handing in project idea | ||||
| +Approval handing in of research proposal | ||||
| Data collection | ||||
| Data Entry | ||||
| Data Analysis | ||||
| Report writing | ||||
| Submission of report | ||||
The prevalence of TB at Twapia clinic was found to be progressively increasing from 2018 at 25% to 40% in 2020, with males being affected more than females and common between the age of 36 to 45 years old. It was noted that 34.3% were coinfected with HIV/TB. With the increase in prevalence, there is need to implement screening strategies, sensitize and encourage people to always visit hospital care and also to continue strengthening the DOT program. There is need to improve TB prophylaxis administration for those on ART and early diagnosis.
The limitations to the study were
• Some Information of interest was not documented in the files hence limiting the study area of discussion.
• Overwhelming work overload in reviewing files.
• Time to do the study adequately was not enough due to the fact that it had to be done while being committed with clinical work which was tiresome.
• Find a more appropriate way of storing patients files.
• Further studies to be carried on.
• Promotion and implementation of strategies to sensitize of early screening, good house ventilation, avoiding overcrowding and treatment adherence.
Information sheet
My names are Mate Matakala, 5th year student from The Copperbelt University School of Medicine. I am carrying out a research on “Prevalence of Tuberculosis and associated risk factors in Twapia area of Ndola District in Zambia,” This is in partial fulfilment of the training in Bachelor of Medicine and Surgery (MBChB).
Purpose of study
The purpose of this study is to determine the proportion of TB cases, to evaluate the trend of TB to determine associated factors and to determine the proportion of Multidrug Resistance TB cases in Twapia area of Ndola District.
Study procedures
In this study, data on TB cases reported from Twapia area will be collected from registers/information systems at Ndola District Health Office. This will include data on TB cases reported from 2018 to 2020, demographic data on TB patients and MDR TB cases.
Confidentiality
In this study, confidentiality and privacy will be assured. No identity information such names of respondents will be required, codes will however, assigned and information obtained will only be used for research purposes.
Study benefits
There will not be any immediate benefit. However, many people may benefit in future if answers are found to the research question.
Study risks
There are no risks associated with participating in this study.
Voluntariness
Your participation in this study is voluntary and should you choose not to participate, no penalty or injury shall occur to you. You also have the right to withdraw from the study at any point.
If you have any questions or clarification on this research please feel free to contact the main researcher or the secretary of the Research Ethics Committee, TDRC on the following addresses;
None.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Clinical Infectious Diseases: Open Access received 1149 citations as per Google Scholar report