Research Article - (2024) Volume 9, Issue 1
Received: 18-Jun-2023, Manuscript No. JCCT-23-103052;
Editor assigned: 21-Jun-2023, Pre QC No. JCCT-23-103052 (PQ);
Reviewed: 04-Jul-2023, QC No. JCCT-23-103052;
Revised: 27-Dec-2023, Manuscript No. JCCT-23-103052 (R);
Published:
03-Jan-2024
, DOI: 10.37421/2577-0535.2024.9.231
Citation: Hagos, Bsrat Tesfay and Gebru Gebremeskel
Gebrerufael. "Time-to-Death Predictors on Breast Cancer Patients in
Northern Ethiopia: A Retrospective Cross-Sectional Study." J Cancer Clin
Trials 9 (2024): 231.
Copyright: © 2024 Hagos BT, et al. This is an open-access article distributed under the terms of the creative commons attribution license which permits unrestricted
use, distribution and reproduction in any medium, provided the original author and source are credited.
Background: Breast Cancer (BC) is still a global public health issue that affects both industrialized and developing nations. It is the type of cancer that affects women most frequently in sub-Saharan African nations, particularly in Ethiopia. Despite the overwhelming difficulty, Ethiopian researchers have not yet identified the factors linked to mortality. Aside than that, there aren't many studies in this field. Therefore, the main goal of this analysis was to identify the most important factors that contributed to BC patients in Northern Ethiopia having shorter survival times.
Methods: 146 women in Northern Ethiopia who had BC were the subjects of an institutional-based retrospective cross-sectional study design that ran from September 12, 2015, to March 9, 2019. The STATA 14 program was used to conduct the statistical analysis. In order to identify predictors, a log-normal regression model and the Kaplan-Meier curve were both used.
Results: In Northern Ethiopia, the overall death rate prevalence was 18.5%. Retrospective monitoring of the chosen patients lasted an estimated 28.12 months on average. The age range of patients was 23-78 years with a median of 48 years. The multivariable Lognormal model analysis revealed, being distant metastatic ATR=0.52, CI=(0.341, 0.787), regional metastatic (ATR=0.63, (0.423, 0.924)), age (ATR=0.98, 95% CI: (0.968-0.997), baseline tumor size (ATR=0.98, 95% CI: (0.968, 0.996), clinical stage IV ATR= 0.48, 95% CI: (0.297-0.789), illiterate ATR=0.52, 95% CI: (0.325-0.823), and Rural residence ATR=0.68, 95% CI: (0.516-0.904) were found to be critical risk factors of time to death breast cancer patients.
Conclusion: The prevalence fatality rate among BC patients in Northern Ethiopia remains a serious public health issue, the research showed. Being clinical stage IV, distant and regional metastasis, illiteracy education level, baseline tumor size, rural residence, and old Age were discovered to be the most significant risk factors for patients' time to death. As a result, the government and other interested parties must address educational possibilities; raising awareness about the diagnosis of advanced disease and providing helpful advice on screening programs in a timely manner will lower the death rate and increase patient survival.
Breast cancer • Lognormal • Time to death • Predictors • Healthcare
ACSH: Ayder Comprehensive Specialized Hospital; ATR: Adjusted Time Ratio; SPSS: Statistical Package for Social Science
With about 1.7 million new cases and 522,000 deaths due to breast cancer-related complications worldwide in 2012, breast cancer is a global public health issue that affects communities all over the world [1]. Globally, it harms about 5.03% of women [2]. Additionally, it is the most frequently identified distortion in both industrialized and some developing nations among women [3].
However, due to a lack of early detection methods and breast cancer therapy, the death rate from breast cancer is significantly greater in low-income countries than in industrialized nations. It is a specific kind of tumor that begins in the breast cells [4]. This demonstrates that breast cancer is the second most frequent cancer after lung cancer and the fifth leading cause of death from cancer [5]. Between 2000 and 2015, sub-Saharan Africa had the highest global incidence rate of breast cancer (22.4 per 100000).
Ethiopia has one of the highest rates of newly diagnosed cases and breast cancer-related deaths in sub-Saharan Africa right now [6].
Breast cancer is the most common cancer, accounting for 33% of malignancies in women and 23% of cancers overall in Ethiopia, according to the study [7]. It is also the predicted national age for women; the standard incidence rate was about 43 per 100,000 individuals. Breast cancer is the most prevalent cancer in women and one of the top 10 cancers in males, according to newly released, preliminary statistics from Addis Abeba city populationbased cancer record. At the Tikur Anbessa specialized hospital, the only hospital in the nation where breast cancer patients could access oncology therapy, the incidence of the disease has shown a stable yearly progression [8,9]. Additionally, 67% of patients present with locally progressed cancer, and 25% with metastatic disease. And this indicating that the majority of patients had advanced disease at the time of presentation [10].
Unsatisfactory treatment outcomes are brought on by the interaction of all the aforementioned reasons [11]. The Ethiopian government has identified this as a significant challenge issue and given improving cancer care in the nation top attention. The cancer controller strategy was formed by Ethiopian healthcare professionals in 2015 and focuses on both prevention and the general advancement of cancer care in the nation [12,13]. The establishment of six specialized cancer health clinics at the Ayder Comprehensive Specialized Hospital (ACSH) in Mekelle, teaching university hospitals in Gondar, Hawassa, Jimma, Haramaya, and St. Paul's hospital was one of the most significant steps made [14]. However, despite a strategy and intention to open more facilities, Ethiopia only has one radiation treatment facility, the Tikur Anbessa comprehensive specialized hospital, located in the nation's capital, and a very small number of chemotherapy facilities throughout. There aren't many researches in Ethiopia that used BC survival analysis. Therefore, it is yet unknown how long BC patients will live on average. Therefore, the goal of this study was to identify the key predictive characteristics that contributed to BC patients' shorter survival times.
Study area and period
Between September 12, 2015, and March 9, 2019, 146 female patients at ACSH in Ethiopia participated in this retrospective cohort study. In the regional state of Tigray, this is the sole public health facility with an oncology unit for the treatment of cancer. The main predictors of survival time-to-death for BC patients were identified by this study. Mekelle, the capital of the Tigray national regional state, is located 783 kilometers from Addis Ababa, the capital of Ethiopia.
Study population
The target population for this study included all BC patients who were admitted to the oncology wards treatment service in ACSH, Tigray regional state, Ethiopia. The individual population consisted of patients receiving treatment from September 12, 2015, to March 9, 2019, in ACSH. The study comprised BC patients who were older than 18 and met the inclusion and exclusion requirements.
Inclusion and exclusion criteria
Women with newly diagnosed adult breast cancer who were enrolled at ACSH at the time of the trial were all included. Women who were on medical recode charts, those who had previously been diagnosed with breast cancer, patients who received a diagnosis at another facility and were subsequently referred to ACSH for additional treatment were all excluded from the study.
Sampling technique and sample size determination procedure
In this study, a specific population percentage approach was used to establish the sample size, and the necessary sample size was computed using the following assumptions; desired precision (d)=5%, the confidence level of significance=95% (Zα/2=1.96) and 45.6% of the prevalence of breast cancer self-diagnosis training between women’s health extension employees in Wolaita zone of Southern Ethiopia was taken [15]. Therefore, the determined sample size by considering a 10% non-response rate was 146. First, all female hospital patients were identified from each medical chart in order to compile the data. Then, a simple random sampling approach was used to choose the samples, employing a lottery method based on the percentage of female patients in each medical chart.
Study variables
Time to death, which was separated into censored and death outcomes and quantified in months, was the main outcome variable. Breast cancer patients who had transferred out at the end of the research period, were alive, and had not been followed up on are referred to as censored. The goals of this inquiry were taken to be right-censored, especially the times for the breast cancer patients who passed away treated as event times and other results. The number of months between a patient's diagnosis and death from breast cancer, the end of the study for patients who were still living, or the date of loss to follow-up is referred to as the patient's survival time.
The number of months between a patient's diagnosis and death from breast cancer, the end of the study for patients who were still living, or the date of loss to follow-up is referred to as the patient's survival time. Additionally, Table 1 displays the predictor factors employed in this investigation.
| Predictor variables | Categories of covariates |
|---|---|
| Age in years | Continuous |
| Baseline hemoglobin level | Continuous |
| Baseline tumor size | Continuous |
| Education level | 0=Tertiary, 1=Secondary, 2=Primary, 3=Illiterate |
| Marital status | 0=Single, 1=Married, 2=Divorced, 3=Widowed |
| Residence | 0=Urban, 1=Rural |
| Clinical stage | 0= stage i, 1= stage ii, 2=stage iii, 3=stage iv |
| Metastasis | 0=Locally, 1=Regional, 2=Distant |
| Baseline treatment | 0=Surgery, 1=Chemotherapy, 2=Chemotherapy and surgery |
Table 1. Description of independent variables.
Statistical data analysis
The statistical program STATA version 14 was used to conduct the statistical analysis. For categorical predictor variables, Kaplan- Meier estimators were employed to show the survival experience of patients through time. The proportion, frequency, and numbers of the patients in relation to all factors were described using descriptive statistics. In order to determine the risk factors for time-to-death patients in this investigation, five parametric survival models (Weibull, Exponential, Log-Logistic, Lognormal, and Gompertz) were fitted. The Akaike Information Criteria (AIC), Bayesian Information Criteria (BIC), and log-likelihood criteria were used to choose the optimal model. Bi-variable and multivariable analyses were done for all predictor variables and those variables with a P-value <0.25 were entered into multivariable parametric survival model analysis [15,16]. Variables having P-value <0.05 in the multivariable model were considered significantly associated with the response variable. Adjusted Time Ratio (ATR) with its 95% Confidence Interval (CI) was computed to show the strength of the association.
Kaplan-Meier estimation
A nonparametric method called Kaplan-Meier (K-M) is used to estimate how long patients will live. It is possible to compare the survival records of two or more groups of patient predictors on an equal footing. It is expressed as the survivor function of Ѕ (t).
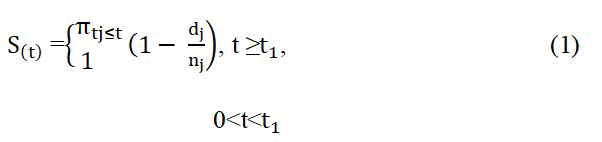
Where, d(j) is the number of patients who experience the event at a time t(j), and, n(j) is the number patients [17].
Lognormal model
One of the parametric survival models that are most frequently employed is one that uses the lognormal distribution. In the study of the survival time dataset, it is crucial. A continuous probability distribution of a random variable that has a normally distributed logarithm is also included. The probability density functions of the lognormal distribution with parameters μ, α, and support random variable x [18].
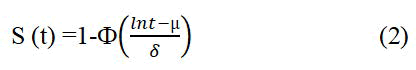
The hazard function is h (t)=f (t)/S (t), Where,
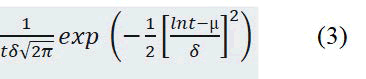
Ѕ (t) is the survival function and Ф (.) is the standard normal distribution function.
Model selection criteria
In this study, many evaluation factors will be taken into account in order to choose the optimal parametric model for simulating breast cancer patients' survival. AIC and BIC [19] were taken into consideration for this work in order to have an adequate model selection for the bi-variable and multivariable parametric survival models.
AIC=-2 × (likehood)+2 × k (4)
BIC=-2 × (likehood)+(N) × k (5)
Where; k is the number of parameters estimated and N is the total number of observations used to fit the model. The Smallest values of AIC and BIC reflect an overall best fit.
Data management
The accuracy of the information collected was guaranteed. The data were analyzed descriptively to provide a summary. Each covariate variable's probability value (P-value) was determined, and a multivariable parametric survival model was created for all covariate variables with a probability value of less than 0.2 in the log-rank test. Based on a probability value (p-value) of less than 0.05 and an Adjusted Time Ratio (ATR) with a 95% confidence interval, statistically significant predictor factors were found.
Demographic characteristics of breast cancer patients
Of the total 146 BC patients (33.1%) and (46.6%), (19.9%) and (33.6%) of them lived in rural and had local, regional, and distant metastasis respectively. On the subject of the clinical stage; (24%), (26.0%), (30.1%) and (19.9%) of breast cancer patients were in stages I, II, III, and IV respectively. Regarding baseline treatment (48.6%), (38.4%), and (13.0%) of breast cancer patients had taken surgery, chemotherapy, chemotherapy, and surgery types of treatment. The age range of BC patients was 23-78 years with a median of 48 years (Table 2).
| Variable | Status of last visit | Frequency (n=146) | Percent (%) | ||
|---|---|---|---|---|---|
| Educational level | Censored | Death | |||
| Illiterate | 7 | 8 | 15 | 10 | |
| Primary | 41 | 9 | 50 | 34 | |
| Secondary | 44 | 6 | 50 | 34 | |
| Tertiary | 27 | 4 | 31 | 21 | |
| Marital status | |||||
| Single | 13 | 2 | 15 | 10 | |
| Married | 71 | 14 | 85 | 58 | |
| Divorced | 21 | 6 | 27 | 19 | |
| Widowed | 14 | 5 | 19 | 13 | |
| Residence | |||||
| Urban | 60 | 10 | 70 | 48 | |
| Rural | 59 | 17 | 76 | 52 | |
| Clinical stage | |||||
| Stage I | 21 | 5 | 26 | 18 | |
| Stage II | 32 | 5 | 37 | 25 | |
| Stage III | 44 | 8 | 52 | 36 | |
| Stage IV | 22 | 9 | 31 | 21 | |
| Metastasis | |||||
| Locally | 70 | 10 | 80 | 55 | |
| Regional | 41 | 11 | 52 | 36 | |
| Distant | 8 | 6 | 14 | 10 | |
| Baseline treatment | |||||
| Surgery | 64 | 14 | 78 | 53 | |
| Chemotherapy | 32 | 36 | 25 | ||
| Chemotherapy and surgery | 23 | 32 | 22 | ||
| Variable | Mean | Median | SD | Minimum | Maximum |
| Age | 48.32 | 48 | 13.6 | 23 | 78 |
| Survival time | 28.12 | 30 | 7.75 | 10 | 36 |
| B_HGL | 13.54 | 13.45 | 1.69 | 10 | 16.2 |
| B_tumor size | 13.42 | 12 | 9.58 | 2 | 37 |
Table 2. Socio demographic characteristics of BC patients in Ayder comprehensive specialized hospital (R version 3.61) the descriptive statistics was explanation.
Comparison of the survival ability of patients
According to the Kaplan-Meier survivor curve estimate, patients with distant and localized metastatic breast cancer had shorter survival times than those who had the disease locally. Compared to tertiary patients, illustrate patients' survival times were shorter according to the the Kaplan-Meier survival estimates curve (Figures 1 and 2). More generally from the log-rank test, there was a significant difference between education level (P=0.001) and metastasis (P=0.0202) in the survival time of breast cancer patients on treatment follow-up (Table 3).
| Variables | Chi-Square | df | Log rank p-value |
|---|---|---|---|
| Education levels | 17.73 | 3 | 0.001 |
| Marital status | 1.32 | 3 | 0.7252 |
| Residence | 2.1 | 1 | 0.1472 |
| Stage | 6.02 | 3 | 0.1106 |
| Metastasis | 7.8 | 2 | 0.0202 |
| Baseline treatment | 3.89 | 2 | 0.1429 |
Table 3. Survival experience comparison.
Model comparison
The study compared various parametric survival models using the information criterion. The researchers employed the AIC and BIC model selection techniques for each model study. The value of AIC and BIC are computed as;
AIC=-2*ln(likelihood)+2*k, and BIC=-2*ln(likelihood+ln(N)*k)
Where; k=The number of parameters estimated, and N=the number of observations. According to the following statistics result of the AIC, BIC, and log likelihood criteria the lognormal regression parametric survival model was preferable for modeling since the lowest value is preferable. This indicates that in terms of relative efficiency and parameterization, the lognormal model is the best efficient for predicting the survival of breast cancer patients (Table 4). Additionally, the survival probability plot of the five parametric survival models shows that the lognormal distribution performs better since it has a distinct step function in comparison to the other distributions, which also explains why the AIC and BIC results are as they are (Figure 3).
| Model | LR | AIC | BIC |
|---|---|---|---|
| Lognormal | -44.8743 | 127.7486 | 184.4371 |
| Weibull | -45.1667 | 128.3333 | 185.0219 |
| Loglogistic | -45.8604 | 129.7209 | 186.4094 |
| Gompertz | -47.2363 | 132.4726 | 189.1611 |
| Exponential | -62.5004 | 161.0008 | 214.7057 |
Table 4. Model comparison.
Predictors of time to death among breast cancer patients
The multivariable analysis of risk predictors associated with time to death was presented in Table 5. The result showed that age, baseline tumor size, level of education, residence, clinical stage, and metastasis were statistically significant predictors of time to death among breast cancer patients. The probability of survival time for breast cancer patients with clinical stage IV was 0.48 times lower than those patients who were clinical stage-I (ATR=0.48, CI (0.297, 0.789*). The risk of death for patients whose distant and regional metastatic was about 0.52-fold and 0.63 times higher than those patients whose local metastasis (ATR=0.52, CI=(0.341, 0.787)*, ATR=0.63, (0.423, 0.924*) respectively. The scale parameter of the lognormal distribution was found to be δ=0.48 with 95% CI (0.363-0.641). This interval does not include δ=1.0 suggesting that the lognormal model is more appropriate than other parametric survival models. Since δ=0.48 which is less than 1, as survival time increases death ratio of breast cancer patients decreases.
| Variables | Crude TR (95% CI) | Adjusted TR (95% CI) |
|---|---|---|
| Age | 0.99 (0.974, 1.00) | 0.98 (0.968, 0.997)* |
| Base HGL | 1.0 (0.922,1.128) | 0.96 (0.879, 10.46) |
| Baseline tumor size | 0.98 (0.964, 0.995)* | 0.98 (0.968, 0.996)* |
| Education (Ref=tertiary) | ||
| Secondary | 0.91 (0.554, 1.490) | 0.73 (0.46, 1.139) |
| Primary | 0.82 (0.513, 1.301) | 0.64 (0.408, 1.01) |
| Illiterate | 0.42 (0.250, 0.704)* | 0.52 (0.325, 0.823)* |
| Marital status (Ref=Single) | ||
| Married | 0.85 (0.464, 1.543) | 1.1 (0.546, 2.031) |
| Divorced | 0.71 (0.361, 1.400) | 0.90 (0.426, 1.88) |
| Widowed | 0.64 (0.313, 1.325) | 0.93 (0.403, 2.151) |
| Residence (Ref=Urban) | ||
| Rural | 0.71 (0.507, 1.00) | 0.68 (0.516, 0.904)* |
| Clinical stage (Ref=Stage I) | ||
| Stage II | 1.3 (0.732, 2.124) | 1.0 (0.636, 1.581) |
| Stage III | 1.2 (0.724, 1.937) | 0.73 (0.431, 1.232) |
| Stage IV | 0.74 (0.447, 1.226) | 0.48 (0.297, 0.789)* |
| Metastasis (Ref=Locally) | ||
| Regional | 0.73 (0.499, 1.056) | 0.63 (0.423, 0.924)* |
| Distant | 0.53 (0.335, 0.839)* | 0.52 (0.341, 0.787)* |
| Baseline treatment (Ref=Surgery) | ||
| Chemotherapy | 1.2 (0.759, 1.953) | 1.3 (0.900, 1.99) |
| Chemotherapy and surgery | 0.77 (0.511, 1.145) | 0.84 (0.600, 1.179) |
| Constant value | 771.7 (124.7, 4774)* | |
| Sigma | 0.48 (0.363,0.641)* | |
Table 5. Multivariable analysis of associated factors of female patient’s in Ayder comprehensive specialized hospital, Mekelle city, Ethiopia.
A retrospective cohort research approach was used in the current analysis. From 146 breast cancer patients, there were 27 fatalities; the mortality prevalence density was about 18.5% per 100. In this study, most of the death of breast cancer patients presented with advanced breast cancer disease (stage IV). The independent predictor variables of illness and death were a clinical stage, metastasis, residence, baseline tumor size, education level, and age had a statistically significant effect on survival time-to-death. In the current study, the overall median survival time for histologically confirmed BC was 30 months.
Breast cancer patients with older women have shorter survival times than those with younger women. This recent study was in conflict with [20], which discovered that BC primarily affects young pre-menopausal women. This outcome was consistent with findings from other studies, which revealed that shorter survival times were associated with older BC patients. The observed difference in mortality rates might be due to the fact that the more advanced stage-IV breast cancer patients were presented in our findings. The same line of results was presented by a different study conducted. This shows that the advanced stage had the greatest impact on patient outcomes in the current study and was a strong predictor of shorter survival time among BC patients. Patients who had distant and regional metastasis had a higher risk of dying than those who only had local metastasis, which was found to be strongly correlated with survival time to death. The patient's chance of survival is decreased when cancer has metastasized, according to earlier studies. This study will help policymakers advocate for better treatment of breast cancer patients. Additionally, this investigation will be used as a jumping off point for additional investigations.
Women in this study with illiterate educational status had much more issues than women with primary, secondary, or tertiary education, according to analysis of the survival time-to-death. According to several studies, education is positively correlated with survival time to death. Others, however, discovered no correlation. This figure may have developed as a result of the lack of mental healthcare and patients' lack of financial knowledge. Patients from the rural residence were highly associated with less survival time ATR: 0.68, 95% CI:(0.516-0.904). This study was similar to other studies conducted in Ethiopia. The findings demonstrate that BC patients from urban regions have higher survival rates than patients from rural locations. Finally, it has been discovered that the initial tumor size significantly affects the amount of time till death. The results of this investigation support.
The prevalence fatality rate among BC patients in Northern Ethiopia remains a serious public health issue, the research showed. Being clinical stage IV, distant and regional metastasis, illiteracy education level, baseline tumor size, rural residence, and old Age were discovered to be the most significant risk factors for patients' time to death. As a result, the government and other interested parties must address educational possibilities; raising awareness about the diagnosis of advanced disease and providing helpful advice on screening programs in a timely manner will lower the death rate and increase patient survival.
BT made contributions on conceptualized the research problem, planned the study, performed statistical model analysis, interpretation of data and revised and drafting the manuscript. GG was involved in, the revision of the research plan, statistical data analysis, and revision of the manuscript for publication. Both authors read and approved the final manuscript.
Not applicable.
The authors declare that there is no competing interest.
The data will be obtained based on the request from the corresponding author of the study.
Not applicable.
Ethical clearance was obtained from Gondar university, college of natural and computational sciences, ethical clearance review committee namely (Dr Bewuket Mehari, Tilahun Yohans, Endalkachew Bizualen, and Tigist Jiginaw) with protocol number: CNCS/10 378/05/2019. Written informed consent was waived by Gondar University, college of natural and computational sciences ethic committee. This study didn’t impose/exposes patients to unnecessary risk as a result of reviewing their medical records. Confidentiality of dataset was kept at all levels of the study and the dataset wasn’t used for other purposes other than for this study. All experiments were performed in accordance with the declaration of Helsinki relevant guidelines and regulations.
Not applicable.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Journal of Cancer Clinical Trials received 95 citations as per Google Scholar report